Every year, thousands of children end up in emergency rooms because someone gave them the wrong dose of an over-the-counter allergy medicine. Not because the medicine is dangerous - but because pediatric antihistamine dosing is confusing, inconsistent, and often done with kitchen spoons. Parents aren’t careless. They’re trying their best. But when the label says “1 teaspoon” and your measuring cup holds 7 milliliters instead of 5, you’re giving your child almost 40% more medicine than intended. That’s not a mistake - it’s a medical emergency waiting to happen.
Why First-Generation Antihistamines Like Benadryl Are Risky for Kids
Diphenhydramine, the active ingredient in Benadryl, has been around since the 1940s. It works fast. It calms itching. It helps with sleep. But for young children, it’s like playing Russian roulette with their nervous system. The gap between a helpful dose and a dangerous one is tiny - just 2:1. That means if your child weighs 22 pounds and needs 9.3 milligrams, giving them 18.6 milligrams could cause seizures, slowed breathing, or even cardiac arrest. The American Academy of Pediatrics (AAP) says it plainly: don’t use diphenhydramine for routine allergies in kids under 2. And even for older kids, it’s not the first choice anymore. Why? Because second-generation antihistamines like cetirizine (Zyrtec) and loratadine (Claritin) are safer. Their therapeutic index - the safety buffer between effective and toxic doses - is 10:1. That’s five times wider. They don’t cause drowsiness. They don’t mess with heart rhythms. And they’re dosed once a day, which cuts down on mistakes. Yet, diphenhydramine still accounts for 83% of emergency visits linked to pediatric antihistamine use, according to Nationwide Children’s Hospital data. That’s not because it’s more popular - it’s because it’s more dangerous when misused.The Measuring Problem: Kitchen Spoons Are Not Medical Tools
The biggest cause of dosing errors? Using a regular kitchen spoon. A teaspoon from your drawer can hold anywhere from 2.5 to 7.5 milliliters. That’s a 300% difference. One parent gives “a teaspoon” of Children’s Benadryl (12.5mg per 5mL) thinking they’re giving 5mL. But their spoon holds 7mL. That’s 17.5mg instead of 12.5mg - a 40% overdose. For a 15-pound toddler, that’s enough to cause dizziness, rapid heartbeat, or vomiting. The FDA required all pediatric liquid medications to come with an oral syringe or dosing cup marked in milliliters since 2011. But a 2018 study in Pediatrics found that 42% of caregivers still use kitchen spoons, cups, or droppers not meant for medicine. Why? Because the instructions say “teaspoon” - and they don’t know that “teaspoon” in medicine means exactly 5mL, not whatever their spoon holds. Even worse, many parents use the same measuring tool for multiple medications. One syringe for Zyrtec, then the same one for Tylenol. No cleaning. No rinsing. That’s how you end up with double doses or wrong concentrations.Understanding Dosing Charts: Weight, Not Age
Age-based dosing is a trap. A 2-year-old weighing 20 pounds and a 2-year-old weighing 30 pounds need completely different amounts. But most labels still say “for ages 2-5.” That’s not safe. Dosing must be based on weight - and even then, guidelines vary. For example:- For a child weighing 20-24 pounds: Diphenhydramine = 9.3mg (¾ teaspoon of 12.5mg/5mL liquid)
- For the same weight: Cetirizine = 2.5mg (½ teaspoon of 5mg/5mL liquid)
- For loratadine: 2.5mg (½ teaspoon of 5mg/5mL liquid)
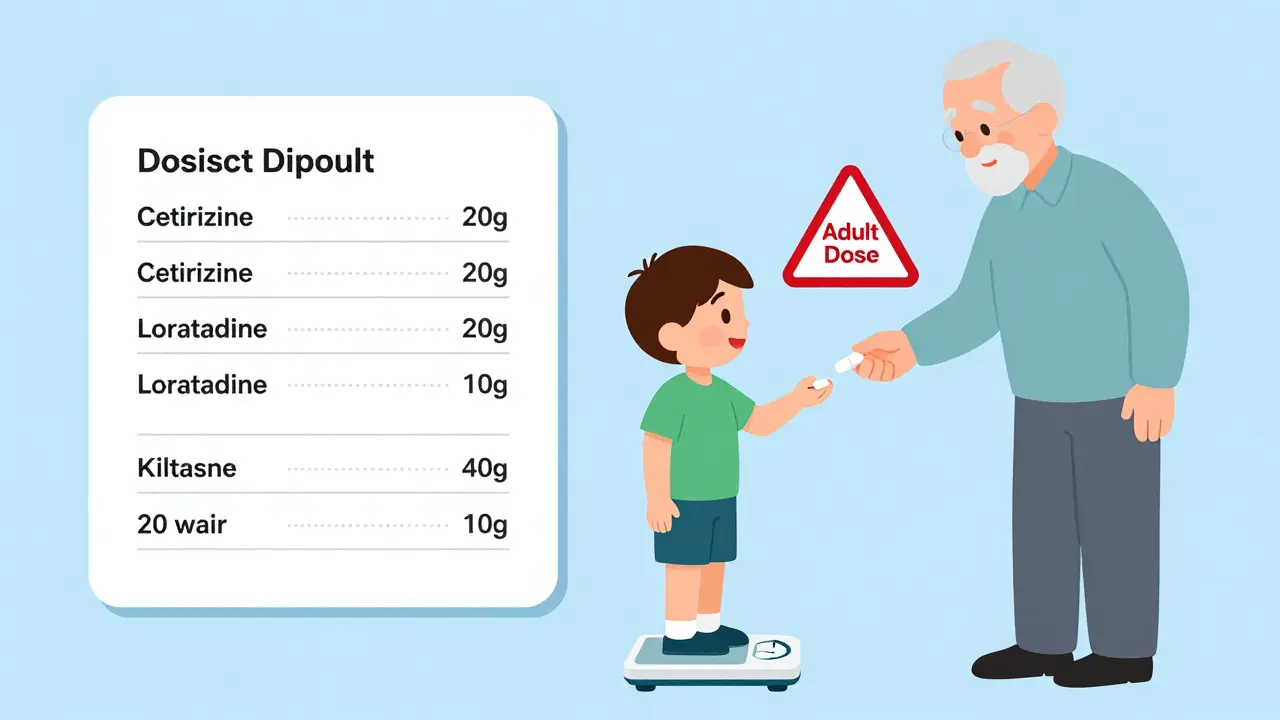
Second-Generation Antihistamines: The Safer Choice
Loratadine and cetirizine aren’t just safer - they’re simpler. Once-daily dosing. Less sedation. Fewer interactions. And because they’re dosed in 2.5mg, 5mg, and 10mg increments, the math is easier. For children 2-5 years old:- Loratadine: 2.5mg daily (½ teaspoon of Children’s Claritin)
- Cetirizine: 2.5mg daily (½ teaspoon of Children’s Zyrtec)
- Loratadine: 5mg daily
- Cetirizine: 5mg daily
How to Get It Right: 5 Steps to Safe Dosing
1. Use only the device that comes with the medicine. That’s the oral syringe or dosing cup. Not a kitchen spoon. Not a medicine dropper from last year. Not a shot glass. Use what’s in the box. 2. Always dose by weight, not age. Keep a scale in your bathroom. Weigh your child every 6 months. Update your dosing chart. If you don’t know your child’s weight, ask your pediatrician - don’t guess. 3. Never mix medications in the same syringe. Clean the syringe with water after each use. Store it in a labeled bag with that specific medicine. Don’t use one tool for Zyrtec, Tylenol, and cough syrup. 4. Ask your pharmacist to show you how to measure. Don’t just take the bottle. Ask them to demonstrate. Say: “Can you show me how to give this to my 20-pound child?” Most pharmacists will do it for free. And 19% of prescriptions get corrected by pharmacists before they’re even picked up. 5. Use a trusted app. Apps like MedsHelper or the Poison Control app (from AAPCC) let you input your child’s weight and instantly show the correct dose. They even have voice confirmation: “You’re giving 2.5mg of Zyrtec. Is that right?” It’s like having a nurse in your pocket.

My niece had a bad reaction to Benadryl last year. We thought a teaspoon was a teaspoon. Turns out, our kitchen spoon held 7mL. She was dizzy for hours. Never used a spoon again. Always use the syringe now. Scary how easy it is to mess up.
Thanks for laying this out so clearly.
As someone from India where OTC meds are often sold without proper labeling, this post is urgently needed. In many households, parents use whatever spoon is handy - even soup spoons. The idea of QR codes linking to dosing videos? Brilliant. We need this globally, not just in the US.
Also, weight-based dosing should be mandatory on all packaging. Age ranges are a relic.
I didn’t realize how big the gap was between diphenhydramine and cetirizine safety profiles. The 2:1 vs 10:1 ratio is wild. My kid gets Zyrtec now - no drowsiness, no drama. And honestly, I forget to give it sometimes because it’s once a day. That’s a feature, not a bug.
Also, the part about grandparents using old advice? Yeah. My mom still swears by Benadryl for ‘sleeping through the night.’ I just quietly swap the bottle when she’s not looking.
Oh my GOD. We’re letting parents use KITCHEN SPOONS to dose kids? Are we in 1985 or 2025? This isn’t a parenting fail - it’s a SYSTEMIC FAILURE.
Someone needs to slap a warning label on every Benadryl bottle that says: ‘If you don’t use the syringe, you’re basically playing medical Russian roulette.’
And why is this even still a thing? The FDA mandated dosing tools in 2011. FOURTEEN YEARS LATER. Are we all just waiting for a kid to die before we fix this?
Also - Zyrtec is the MVP. Stop being cheap with your child’s brain.
Look - I used to be the guy who gave Benadryl to my kid because it ‘calmed him down.’ I thought it was harmless. Then I read this. I felt like an idiot. But now? I’m the guy who carries the dosing syringe everywhere. I even have a labeled bag for meds. I’m not proud of how ignorant I was - but I’m proud of how I changed.
If you’re still using a spoon, stop. Just stop. Your kid deserves better.
OMG I just realized I used the same syringe for Zyrtec and Tylenol last week 😳 I rinsed it with water but... ugh. I’m so embarrassed. I’m buying a new one today and labeling them like a pro. 🙈 Thanks for the wake-up call!! 💙
The data presented here is methodologically sound. The emphasis on weight-based dosing aligns with the 2023 AAP Clinical Practice Guideline on Pediatric Pharmacotherapy. The 42% kitchen spoon usage statistic, corroborated by the 2018 Pediatrics study, underscores a persistent behavioral gap in caregiver education.
Furthermore, the therapeutic index differential between first- and second-generation antihistamines is not merely statistically significant - it is clinically decisive. The risk-benefit ratio favors cetirizine and loratadine unequivocally.
Recommendation: institutionalize dosing demonstrations in all primary care pediatric visits.
i read this and thought of my cousin in delhi - she gives benadryl to her 2yo every time he sneezes. no idea what the dose is. just a spoon. i showed her this post. she said ‘but it worked for me as a kid’... sigh. hope she listens. kids ain’t little adults man.
also zyrtec is way better. no sleepy baby = happy mama.
Wow. A 1,200-word essay on not using a teaspoon. Groundbreaking. Next up: ‘How to Avoid Breathing Air That Contains Oxygen.’
Also, ‘Children’s Benadryl’? What, did they name it that to trick adults into thinking it’s safe? Brilliant marketing. Not brilliant medicine.
Why are we letting Americans be this careless? In my country, you’d be fined for giving a child medicine without a prescription - and even then, the pharmacist walks you through it. We don’t have ‘kitchen spoon culture.’ We have responsibility.
And yet here we are, letting people wing it with their kid’s brain chemistry because ‘it’s just Benadryl.’
It’s not. It’s negligence dressed up as parenting.
Every time I see someone say 'it was fine for me' - I want to scream. My cousin’s daughter had a seizure from Benadryl. She’s 8 now and still has mild tremors. It’s not ‘just a mistake.’ It’s trauma. It’s lifelong.
And no, you don’t get a pass because you ‘didn’t mean to.’
Use the syringe. Dose by weight. Or don’t give it at all.
And if you’re still using Benadryl for sleep? You’re not a parent. You’re a liability.
It is imperative to underscore the salient clinical distinction between first-generation and second-generation antihistaminergic agents with respect to their pharmacokinetic profiles, particularly regarding blood-brain barrier permeability and muscarinic receptor affinity.
Moreover, the non-adherence to standardized dosing protocols - particularly the continued reliance on volumetric approximations via non-calibrated household utensils - constitutes a critical public health vulnerability, which, if unmitigated, may result in iatrogenic morbidity and increased emergency department utilization.
Recommendation: Implement mandatory, FDA-certified, color-coded dosing devices with integrated, tamper-evident calibration indicators, distributed at point-of-sale, with accompanying QR-linked instructional micro-videos, in all pediatric OTC antihistamine packaging.
Just use the syringe. Weigh your kid. Pick Zyrtec or Claritin. Don’t overthink it.
It’s not about being perfect. It’s about being careful. And if you’re scared you messed up? Call Poison Control. They’ve heard it all. They won’t yell. They’ll help.
That’s it. That’s the whole post.