Every year, over 1.3 million people in the U.S. end up in the emergency room because of problems with their medications. Many of these cases aren’t accidents-they’re preventable. You’re not alone if you’ve ever been confused about when to take your pills, worried about mixing them with other drugs, or wondered if that new bottle looks different from last time. Medication safety isn’t just for doctors and pharmacists. It’s something you need to know, every single day.
Know Your Medications Like Your Phone Number
You wouldn’t trust a stranger to tell you your password. So why trust someone else to explain your meds? Start by making a real, written list of everything you take. Not just prescriptions. Include vitamins, supplements, herbal teas, and over-the-counter painkillers like ibuprofen or antacids. Many people forget these, but they can cause serious reactions. For example, mixing blood thinners like warfarin with garlic supplements can increase bleeding risk. The CDC says half of all medication errors happen during care transitions-like leaving the hospital or switching doctors-because no one had the full picture.Update this list every time you see a provider. Bring it with you. Don’t rely on memory. Write down the name, dose, why you’re taking it, and how often. If you take ten pills a day, write it out. If you take insulin, write the exact type and amount. Keep it in your wallet or save it on your phone. A simple list cuts your risk of a dangerous mix by up to 40%.
The Five Rights of Safe Medication Use
Healthcare workers use the "Five Rights" to avoid mistakes. You should too:- Right patient - Is the name on the bottle yours? Double-check spelling.
- Right drug - Does it match your list? Look up the pill shape and color if you’re unsure.
- Right dose - Is it 5 mg or 50 mg? Don’t guess. Read the label twice.
- Right route - Is it meant to be swallowed, injected, or applied to the skin? Never crush a pill unless your doctor says it’s okay.
- Right time - Take it at the same time every day. Use alarms on your phone. Missing doses or taking too much can be just as dangerous.
These aren’t just hospital rules. They’re your personal safety checklist. If you’re ever unsure, pause. Don’t take it. Call your pharmacist. They’re trained to catch what others miss.
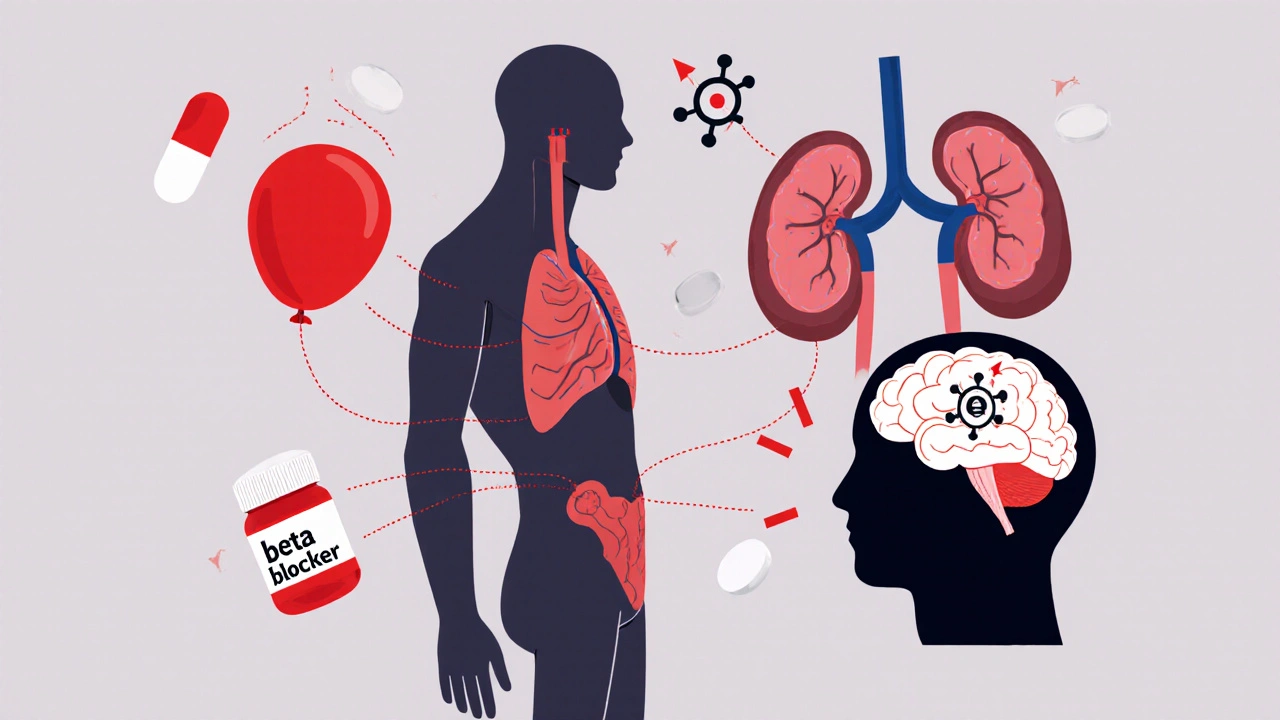
Watch Out for High-Risk Drugs
Some medications are more dangerous if used wrong. These are called "high-alert" drugs. They include:- Insulin - too much can crash your blood sugar fast
- Warfarin - a blood thinner that needs regular testing
- IV heparin - used in hospitals, but can cause severe bleeding if dosed wrong
- IV oxytocin - used during labor, but mistakes can lead to uterine rupture
These drugs account for nearly one-third of all serious medication errors. If you’re prescribed one, ask: "Why is this high-risk? What happens if I take too much? What signs should I watch for?" Your pharmacist can show you how to recognize early warning signs-like unusual bruising, dizziness, or confusion. Don’t wait for a crisis. Learn the red flags now.
Ask the FDA’s Eight Questions
When a new prescription comes in, don’t just take it. Ask these eight questions. Write them down if you need to:- What’s the name of this medicine?
- What’s the active ingredient? (Some brands have the same one.)
- Why am I taking this?
- How much should I take, and when?
- What should it look like? (Color, shape, markings.)
- When does it expire?
- What are the most common side effects?
- What should I avoid? (Alcohol? Other meds? Foods?)
- What if I miss a dose?
Studies show patients who ask these questions remember 50% more about their meds. If your provider brushes you off, find another. Good care means clear answers.
Look-Alike, Sound-Alike Drugs Are a Silent Killer
Glimepiride. Glyburide. Prednisone. Prednisolone. These names sound almost identical. But they treat very different things. One lowers blood sugar. The other reduces swelling. Taking the wrong one can land you in the hospital.Over 60% of pharmacy errors involve look-alike or sound-alike drugs. The fix? Tall Man Lettering. That’s when drug names are written with mixed capitalization to highlight differences: predniSONE vs. predniSOLONE. You won’t always see it on your label, but you can protect yourself. Always check the exact spelling on the bottle. Compare it to your old prescription. If it looks different, ask. A Reddit user shared how they took the wrong diabetes pill for three days-until their blood sugar crashed. That could’ve been avoided.

Don’t Guess. Don’t Skip. Don’t Stop.
Many people stop taking antibiotics early because they feel better. That’s dangerous. The FDA says 23% of antibiotic failures happen because people quit too soon. Same with blood pressure meds. If you feel fine, you might think you don’t need them anymore. But that’s when they’re working.Never skip doses. Never double up if you miss one. Call your doctor or pharmacist instead. They’ll tell you what to do. If you can’t afford your meds, ask about patient assistance programs. Don’t cut pills in half unless it’s approved. Some pills are designed to release slowly-cutting them ruins the effect.
Use Tools That Actually Work
Pill organizers? They help. Especially for older adults. One study found they reduce errors by 35%. But only if you fill them correctly. Set phone alarms. Use apps like the CDC’s new Medication Safety Checklist (launched in January 2024). It lets you scan your pills, log doses, and get reminders.For people taking five or more meds, the risk of error jumps 3.2 times. That’s why simple tools matter. A pill box with days of the week. A sticky note on the fridge. A voice reminder: "Take your metformin." These aren’t childish-they’re lifesaving.
When You’re in Transition, Be Extra Careful
Leaving the hospital? Switching doctors? Moving to a new pharmacy? These are the most dangerous times for medication errors. Hospitals are supposed to do medication reconciliation-comparing your current list with what you’re being prescribed. But only 58% of U.S. hospitals consistently record over-the-counter meds and supplements. That’s a gap.Take control. Before you leave the hospital, ask: "Can I get a printed list of everything I’m supposed to take now?" When you see your new doctor, bring your list. Don’t assume they’ll know what you were on. If you’re using telehealth, make sure the provider has your full history. Telehealth errors jumped 200% during the pandemic because records weren’t shared properly.
Get Help From Your Pharmacist
Your pharmacist isn’t just the person who hands you the bottle. They’re trained to catch errors, spot interactions, and explain your meds in plain language. Yet, most people never ask them questions.When you pick up a new prescription, ask: "Is this safe with my other meds?" "Are there cheaper options?" "What should I do if I feel weird after taking it?" Patients who talk to pharmacists have 27% fewer mistakes. Many pharmacies offer free med reviews-just ask. Bring all your bottles. Even the empty ones. They’ll spot duplicates, expired drugs, or dangerous combos.

Clean Out Your Medicine Cabinet
Expired meds? Unused antibiotics? Old painkillers? They’re not just clutter. They’re risks. The Illinois Department of Health says 38% of accidental poisonings in kids happen because of old pills left in cabinets. Even if they’re "just vitamins," they can be dangerous if someone else takes them.Do a medicine cabinet clean-out twice a year. Throw out anything past its expiration date. Don’t flush most pills-check your local pharmacy’s take-back program. Many offer free disposal. If you’re unsure, call your pharmacist. They’ll tell you how to dispose of it safely.
Teach-Back: The Secret to Remembering
Your doctor says, "Take this twice a day with food." Do you really understand? Try this: after they explain, say, "So just to make sure I got it right-you want me to take [name of drug] twice a day, after breakfast and dinner, for [number] weeks, to help with [condition]?"This is called the "teach-back" method. It’s simple, but powerful. A 2021 study found patients who used it had 40% better adherence. It forces you to process the info. It helps your provider know if you’re confused. And it catches misunderstandings before they become mistakes.
It’s Not Just About Taking Pills
Medication safety isn’t just about not mixing drugs or taking the right dose. It’s about knowing your body, asking questions, and speaking up. It’s about trusting your gut-if something feels off, it probably is. You’re the most important person in your own care. No system, no app, no pharmacist can replace your awareness.Start today. Write down your meds. Ask the eight questions. Use a pill box. Talk to your pharmacist. Clean out your cabinet. These aren’t extra steps. They’re your shield.
What should I do if I think I took the wrong pill?
Stop taking it immediately. Call your pharmacist or poison control (1-800-222-1222 in the U.S.). Don’t wait for symptoms. Have the pill bottle with you when you call-they’ll need the name, dose, and barcode. If you’re unsure which pill you took, take a photo and show it to a healthcare provider. Most errors are caught before they cause harm if you act fast.
Can I share my prescription meds with family members?
Never. Even if they have the same symptom. A drug that works for you could be dangerous for someone else. Dosages vary by weight, age, kidney function, and other meds they take. Sharing prescriptions is illegal and can cause serious harm-or death. If someone needs help, they should see their own doctor.
Why do my pills look different this time?
Pharmacies often switch manufacturers, which changes the pill’s color, shape, or markings. That doesn’t mean it’s wrong-but you should always check. Compare the name, dose, and instructions on the label to your previous bottle. If anything looks off, call your pharmacist. Never assume it’s the same drug. Look-alike pills are a leading cause of errors.
How do I know if a medication is expired?
Check the expiration date on the bottle or box. It’s usually printed as month/year. Some pills lose potency after expiration, but others-like insulin or liquid antibiotics-can become dangerous. If you’re unsure, don’t take it. Bring it to your pharmacy for disposal. Most offer free take-back programs. Never use expired meds, even if they look fine.
What if I forget to take my pill? Should I double the next dose?
Never double up unless your doctor says so. For most medications, if you miss a dose, take it as soon as you remember-if it’s not close to the next scheduled dose. If it’s almost time for the next one, skip the missed dose. Taking too much can be deadly, especially with blood thinners, insulin, or heart meds. Always check the instructions or call your pharmacist for guidance.
Are natural supplements safe to take with my prescriptions?
Not always. Supplements like St. John’s Wort, ginkgo, garlic, and vitamin E can interfere with blood thinners, antidepressants, and blood pressure meds. Many people think "natural" means safe, but that’s not true. Always tell your doctor and pharmacist about every supplement you take-even if you think it’s harmless. They can check for interactions you didn’t know existed.
How often should I update my medication list?
Update it every time you see a doctor, pharmacist, or hospital. Also update it after any new prescription, change in dose, or if you stop a medication. Keep a digital copy on your phone and a printed version in your wallet. Many hospitals now require you to bring your list to every visit. Don’t wait for them to ask-be ready.
Can I trust my doctor to catch all medication errors?
Doctors are human. They see dozens of patients a day. Even with electronic systems, mistakes happen. That’s why you need to be your own advocate. Use your medication list, ask questions, and verify everything. Pharmacists are trained specifically to catch these errors-they’re your second line of defense. Don’t rely on one person to get it right. Build a safety net with multiple checks.
What Comes Next?
If you’re managing multiple medications, start small. Pick one habit: write your list. Or ask your pharmacist one question next time you pick up a prescription. That’s enough to start reducing risk. Over time, these small steps become routines-and routines save lives.Medication safety isn’t complicated. It’s consistent. It’s asking. It’s checking. It’s speaking up. You don’t need to be a doctor to keep yourself safe. You just need to care enough to pay attention.


This is the kind of post that should be mandatory reading for every adult. I used to ignore my meds until my grandma ended up in the ER over a supplement interaction. Now I keep a laminated list in my wallet. Simple, but it saved my life.
Stop treating your prescriptions like a game of chance. You wouldn’t drive without a seatbelt-why risk your body like this?
YAS. 🙌 I use the CDC app and set 4 alarms a day. My mom thinks I’m obsessive but when you’re on 7 meds including warfarin, you don’t get to wing it. Also, ALWAYS check the pill shape. Last month I almost took a generic that looked identical but had a different release profile. Pharmacist caught it. She’s my hero.
Also-stop hoarding expired antibiotics. I found my ex’s leftover cipro in a sock drawer. That’s not storage. That’s a biohazard.
PS: I use emojis because I’m not a robot. Deal with it. 😎
Look, I appreciate the effort here, but let’s be real-this is all just corporate wellness fluff dressed up as medical advice. The system is broken. Pharmacies are understaffed, doctors are overworked, and patients are treated like data points. You can list the Five Rights all day, but if your insurance won’t cover your insulin, or your pharmacist can’t answer your call because they’re juggling 200 scripts, none of this matters. The real issue isn’t that people don’t know how to take pills-it’s that they’re forced to take them in a system designed to fail them. Stop putting the burden on the patient. Fix the infrastructure.
Also, ‘teach-back’? That’s a buzzword. I’ve had doctors ask me to repeat instructions like I’m a toddler. It’s patronizing, not empowering.
And don’t get me started on ‘natural supplements.’ You know what’s natural? Being born without a prescription. But no, we’re told to treat our bodies like broken machines needing constant software updates.
Just saying. I’m not against safety. I’m against performative safety that ignores systemic failure.
Oh my god. I just realized I’ve been taking my metformin with coffee for two years. I thought it was fine because I didn’t feel sick. But now I’m wondering-was my ‘normal’ just my body slowly dying? This post made me cry. Not because I’m dramatic, but because I’m terrified I’ve been doing this wrong for so long.
I used to think asking questions made me annoying. Now I know it’s the only thing keeping me alive. I called my pharmacist today. She spent 20 minutes going over my list. I cried again. Not from sadness-from relief.
Thank you for writing this. Not everyone gets it. But I do now.
And yes, I cleaned out my cabinet. Threw out 17 expired bottles. Including that ‘emergency’ Xanax from 2018. I’m never doing that again.
While the post’s heuristic framework is laudable, it fundamentally misrepresents the epistemological hierarchy of pharmaceutical stewardship. The ‘Five Rights’ model is a pre-20th century operational schema, insufficient for the ontological complexity of polypharmacy in the post-industrial pharmacopeia. The reliance on patient self-reporting as a primary safeguard is a classic case of misplaced agency-what we require is algorithmic reconciliation via blockchain-integrated EHRs, not sticky notes.
Moreover, the normalization of ‘pill organizers’ as a clinical intervention betrays a profound misunderstanding of cognitive load theory. A neurodivergent patient managing 12 medications requires a digital twin, not a plastic tray.
And while I applaud the emphasis on pharmacist consultation, the structural barriers-reimbursement models, corporate pharmacy consolidation, and the commodification of clinical expertise-render this advice functionally inert. You cannot empower the patient if the system is engineered to disempower them.
TL;DR: Awareness is necessary but insufficient. We need systemic reengineering, not behavioral nudges.
Everyone’s acting like this is groundbreaking. It’s not. This is just a list of things you learn in med school 101. You don’t need a 2000-word essay to tell people to read the label. Also, who cares if your pills look different? That’s literally how generics work. You’re overcomplicating a basic life skill.
And ‘teach-back’? That’s just a fancy way of saying ‘repeat after me.’ I’ve had nurses do that to me like I’m a dog. It’s humiliating.
Also, the CDC app? It’s clunky. And don’t get me started on ‘natural supplements.’ Half the people who take them are just trying to feel better without seeing a real doctor. You’re enabling that mindset by treating supplements like they’re on the same level as prescription drugs.
Stop making people feel guilty for being human. We’re all tired. We forget. We mix things up. It happens. The system should adapt, not punish us for it.
Hey, if you’re reading this and you’re scared-good. That means you’re paying attention. I used to be the person who skipped doses because I felt fine. Then I had a heart scare. Now I use a pill box, set alarms, and call my pharmacist every time I get a new script. It’s not hard. It’s just consistent.
You don’t have to be perfect. Just show up. Write one thing down. Ask one question. That’s enough to start.
You’re not a burden. You’re not annoying. You’re the most important person in your own care. And you deserve to be safe.
I believe in you. Keep going.
Thank you for this. 🙏 I’m 72 and on 9 meds. I used to forget which was which until I started taking a photo of my pill box every morning. I send it to my daughter. She checks it. I feel less alone.
Also-I asked my pharmacist about the garlic supplement I was taking for ‘heart health.’ Turns out it was thinning my blood too much. She gave me a list of safe alternatives. She didn’t judge me. She helped me.
Don’t be embarrassed to ask. We’re all learning. And if you’re reading this and you’re overwhelmed-take a breath. You’ve got this. One pill at a time. 💪
so i just found out my blood pressure med changed from blue to white and i thought it was a different drug so i stopped taking it for 3 days and my head was pounding and i was dizzy and i was so scared but then i called the pharmacy and they said oh its just a different manufacturer and i felt so dumb but also like wow why is this so confusing
and now im going to make a list and i think im gonna put it on my fridge with a sharpie and i might cry when i do it but i think its worth it
also i stopped taking my fish oil because i thought it was fine but now im gonna ask my pharmacist next time i see her
thank you for writing this
It is imperative to acknowledge that the efficacy of patient-centered medication safety protocols is contingent upon the integrity of the pharmaceutical supply chain and the regulatory oversight of drug manufacturing. The variance in pill appearance, while ostensibly benign, is symptomatic of a broader deregulatory trend in generic drug production, wherein bioequivalence thresholds are systematically relaxed. This phenomenon, observed across multiple jurisdictions, introduces an unacceptable degree of pharmacokinetic variability.
Furthermore, the assertion that patient self-reporting mitigates error is empirically unsupported. A 2022 JAMA study demonstrated a 68% underreporting rate of OTC supplement use among elderly patients. The reliance on mnemonic devices such as the ‘Five Rights’ constitutes a cognitive band-aid, not a structural solution.
It is therefore recommended that all individuals undergo mandatory pharmacogenomic screening prior to polypharmacy initiation. This would enable personalized dosing algorithms, eliminating human error at its source. Until such time, patient advocacy remains a necessary but insufficient palliative.
Do you think people actually read all this? I’m not being mean-I’m just curious. I feel like this is the kind of thing you save to read later, then forget about. I read it once, then didn’t look at it again. I think the real problem isn’t knowledge-it’s habit. How do you make this stick? How do you turn ‘I should do this’ into ‘I do this every day’?
I’ve tried pill organizers. I’ve tried alarms. I’ve written lists. But I still forget. Or I get lazy. Or I think ‘it’s just one time.’
Is there a way to make this feel less like a chore? Like, something that feels good to do, not just something you feel guilty about not doing?
Emily P asked the real question. We’re not machines. We’re tired. We’re overwhelmed. We’re working two jobs, caring for kids or parents, dealing with anxiety, depression, chronic pain. And now you want us to memorize five rights and scan pills and keep a list and call the pharmacist and clean out our cabinets?
That’s not safety. That’s burnout with a side of guilt.
What if we stopped blaming people for not being perfect and started fixing the system that expects perfection from people who are barely surviving?
I don’t need a checklist. I need a system that doesn’t make me feel like a failure every time I forget to take my pill.
And yes-I still take my meds. But I don’t feel proud of it. I feel exhausted.