What if the medicine you take to control your blood pressure could make your asthma worse? Or if the pill for your diabetes could hide the signs of low blood sugar until it’s too late? These aren’t hypotheticals. They’re real, dangerous, and surprisingly common. Drug-disease interactions happen when a medication meant to help one health problem accidentally makes another one worse. And most people don’t even know they’re at risk.
How a Medicine Can Hurt More Than Help
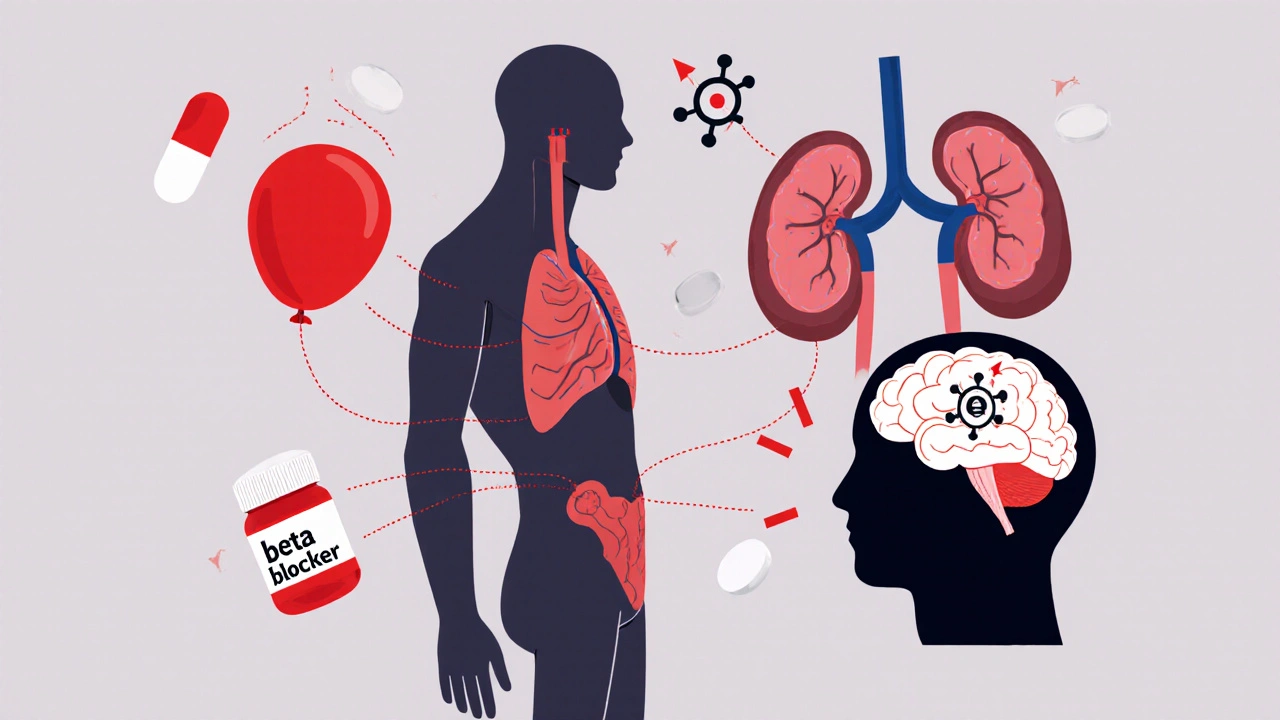
It’s easy to think of medications as simple fixes: take a pill, fix the problem. But your body isn’t a machine with separate parts. It’s one system. When you have more than one chronic condition - and most adults over 65 do - drugs don’t just act on one target. They ripple through your whole physiology. Take beta-blockers, often prescribed for high blood pressure or heart disease. They slow your heart rate and lower blood pressure. Sounds good, right? But if you also have asthma, these same drugs can tighten your airways. That’s not a side effect - it’s a direct conflict. The drug is working exactly as designed, but in the wrong context. The result? Trouble breathing, emergency visits, even hospitalization. Or consider NSAIDs like ibuprofen. They’re common for arthritis pain. But if you have heart failure, they cause your body to hold onto sodium and fluid. That extra fluid pushes harder on your weakened heart. Suddenly, a pain reliever becomes a heart stressor. Even something as simple as a decongestant like pseudoephedrine can be dangerous. It raises blood pressure. If you’re on medication to keep your pressure down, this one cold pill can undo weeks of control. And most patients have no idea.The Five Ways Disease Changes How Drugs Work
Not all drug-disease interactions look the same. They follow five main patterns, each with real-world consequences:- Pharmacodynamic interference: The drug’s effect fights against your disease. Beta-blockers and asthma is one example. Another is using SSRIs for depression if you’re also on lithium - the combination can trigger serotonin syndrome, a life-threatening surge in brain chemicals.
- Pharmacokinetic changes: Your disease changes how your body processes the drug. Liver disease slows down how fast your body breaks down warfarin. That means the blood thinner stays in your system longer, raising your risk of dangerous bleeding - even if you’re taking the same dose as someone with a healthy liver.
- Masking symptoms: The drug hides warning signs. Beta-blockers can stop you from feeling your heart race or sweating when your blood sugar drops. For someone with diabetes, that means a low blood sugar episode can turn into a coma before they even notice.
- Exacerbating complications: The drug worsens an existing problem. Metformin, a common diabetes drug, is normally safe. But if your kidneys aren’t working well, it can build up and cause lactic acidosis - a rare but deadly condition.
- Direct organ toxicity: The drug damages an already fragile organ. Certain antibiotics can harm kidneys already weakened by diabetes or high blood pressure. Even common painkillers can cause liver damage in people with hepatitis or fatty liver disease.
These aren’t rare edge cases. A 2015 analysis found that 84% of serious drug-disease interactions in diabetes patients involved kidney problems. In heart failure, 35% of harmful events were linked to bleeding risks from blood thinners. And depression treatments? Nearly half the risks involved bleeding or lithium toxicity.
Who’s Most at Risk?
You don’t need to be elderly to be at risk. But if you’re over 65, your odds jump. The average American over 65 takes five medications daily and has four chronic conditions. That’s a recipe for conflict. The top four health conditions that create the most dangerous drug-disease interactions are:- Chronic kidney disease: Nearly every drug passes through the kidneys. If they’re damaged, drugs build up. Metformin, NSAIDs, certain antibiotics, and even some heart medications become risky.
- Heart failure: Fluid balance is fragile. Drugs that cause fluid retention - like NSAIDs, certain diabetes pills, or even some calcium channel blockers - can make heart failure worse overnight.
- Liver disease: The liver breaks down most drugs. If it’s scarred or fatty, drugs stick around too long. Warfarin, statins, and even acetaminophen can become toxic.
- Psychiatric conditions: Depression, bipolar disorder, and anxiety often require multiple drugs. Mixing SSRIs with lithium, St. John’s wort, or even certain migraine meds can trigger serotonin syndrome - a medical emergency.
People with these conditions are often prescribed multiple drugs - and each new prescription adds another layer of risk. And here’s the kicker: many doctors don’t screen for these interactions. A 2020 study found that only 16% of clinical guidelines for diabetes, depression, or heart failure even mention drug-disease risks.
Why EHRs and Pharmacies Still Miss These Dangers
You’d think computers would catch this. Electronic health records (EHRs) are supposed to warn doctors when a drug clashes with a condition. But they’re flawed. Epic’s latest system flags 87% of high-risk interactions - but 42% of those warnings are false alarms. That means doctors see a red alert for something harmless 4 out of 10 times. After a while, they stop paying attention. This is called “alert fatigue.” And when that happens, the real dangers slip through. Community pharmacists are often the last line of defense. But they’re rushed. On average, they spend just over 12 minutes per patient reviewing medications. That’s not enough to dig into complex comorbidities. And patients rarely bring up their full medical history unless asked directly. A 2022 survey found only 22% of people with high blood pressure knew why decongestants could be dangerous. Most assume if a drug is sold over the counter, it’s safe. It’s not.What You Can Do to Protect Yourself
You don’t need to be a doctor to reduce your risk. Here’s how to take control:- Keep a full medication list. Include prescriptions, over-the-counter drugs, vitamins, and supplements. Don’t forget herbal products like St. John’s wort - it’s one of the riskiest, with documented cases of serotonin syndrome when mixed with antidepressants.
- Ask your doctor or pharmacist this question: “Could any of these medications make my other conditions worse?” Say it out loud. Write it down. Don’t assume they know your full history.
- Know your kidney and liver numbers. If you have diabetes, heart disease, or high blood pressure, get your creatinine and ALT/AST levels checked yearly. These simple blood tests tell you if your organs can handle your meds.
- Use the Beers Criteria. It’s a list of medications that are risky for older adults with certain conditions. Ask your pharmacist if your meds are on it. The 2023 update added new warnings for anticholinergics in dementia patients and opioids in COPD.
- Watch for hidden signs. If you suddenly feel more tired, swollen, short of breath, or confused after starting a new drug - don’t wait. Call your doctor. It might be a drug-disease interaction.
There’s no magic bullet. But awareness saves lives. A 2021 study at Mayo Clinic showed that a dedicated drug-disease interaction screening program cut hospital readmissions by 27% in just one year.

The Bigger Picture: Why This Isn’t Fixed Yet
The problem isn’t just individual mistakes. It’s systemic. Medical schools spend an average of 4.2 hours teaching drug-disease interactions. That’s less than one lecture. Meanwhile, the FDA now requires new drugs to be tested in patients with common comorbidities - a step forward. The European Medicines Agency now demands a dedicated section in every drug’s label for disease interactions. But in the real world, guidelines still treat diseases in isolation. Diabetes guidelines don’t warn about heart failure risks. Heart failure guidelines don’t flag kidney dangers. And patients are left in the middle. The future lies in personalized medicine. The NIH’s All of Us program is using AI to link genetic data with health records to predict who’s most at risk. Early results show 38% better accuracy than current methods. But until then, the burden falls on you. You’re the only one who knows your full health story. Don’t wait for a system that’s still catching up.When to Seek Help Immediately
Some drug-disease interactions turn dangerous fast. Call 911 or go to the ER if you experience:- Sudden confusion, agitation, or hallucinations (possible serotonin syndrome)
- Severe swelling in legs, ankles, or abdomen (fluid buildup from heart failure worsening)
- Unexplained bruising, bleeding gums, or dark stools (signs of internal bleeding from drug effects)
- Difficulty breathing after starting a new beta-blocker or decongestant
- Extreme fatigue, nausea, or muscle pain with dark urine (possible lactic acidosis from metformin)
These aren’t side effects. They’re red flags. And they’re preventable.
What’s the difference between drug-drug and drug-disease interactions?
Drug-drug interactions happen when two or more medications affect each other - like warfarin and aspirin increasing bleeding risk. Drug-disease interactions occur when a medication worsens an existing health condition, even if no other drug is involved. For example, taking ibuprofen with heart failure isn’t about another pill - it’s about how ibuprofen affects your heart’s ability to manage fluid.
Can over-the-counter medicines cause drug-disease interactions?
Absolutely. Common OTC drugs like ibuprofen, pseudoephedrine, antacids with aluminum, and even some sleep aids can cause serious problems. For example, people with kidney disease should avoid NSAIDs. Those with glaucoma should avoid decongestants. And antihistamines like diphenhydramine can worsen confusion in older adults with dementia. Just because it’s sold without a prescription doesn’t mean it’s safe for your specific health profile.
Are herbal supplements safe if I have chronic conditions?
No. Supplements like St. John’s wort, ginkgo biloba, garlic, and ginseng can interact dangerously with medications. St. John’s wort can cause serotonin syndrome when taken with SSRIs. Ginkgo increases bleeding risk with blood thinners. Garlic can lower blood pressure too much if you’re already on antihypertensives. Always tell your doctor about every supplement you take - even if you think it’s harmless.
How often should I review my medications with a pharmacist?
At least once a year - or anytime you start, stop, or change a medication. If you have three or more chronic conditions or take five or more medications, schedule a medication review every six months. Pharmacists can spot hidden risks that doctors miss, especially when you’re seeing multiple specialists.
Is there a tool I can use at home to check for drug-disease interactions?
Yes. The Beers Criteria is the gold standard for older adults and is available online from the American Geriatrics Society. CredibleMeds.org also offers free resources for patients and caregivers. But remember: tools can’t replace professional advice. Use them to prepare questions for your doctor or pharmacist - not to make decisions on your own.


Wow, this is the kind of post that makes you stop scrolling and actually think. I never realized how dangerous OTC meds could be for people with chronic conditions. My grandma took ibuprofen for her arthritis and ended up in the hospital because of fluid retention - no one ever warned her. 😢
Man, I’ve been there. My dad’s on five meds, has diabetes, heart issues, and kidney trouble. The pharmacists are always rushed, and the doctors act like they’re reading a checklist. But this? This is the real stuff. We need more than algorithms - we need people who actually listen. Thanks for putting this out there. 🙏
Let me tell you something - this isn’t just about medicine, it’s about respect. Your body ain’t a box with separate drawers. It’s one big, messy, beautiful system that’s trying to survive everything you throw at it. Beta-blockers and asthma? Yeah, that’s a nightmare waiting to happen. NSAIDs and heart failure? Same thing. And don’t even get me started on how we treat supplements like candy. St. John’s wort? That’s not herbal tea, that’s a chemical grenade. But here’s the good part: you can fight back. Keep a list. Ask the damn question. Get your kidney numbers checked. You don’t need a PhD to save your life - just a little awareness and the guts to speak up. This post? It’s a lifeline. Pass it on. 🌍❤️
THIS IS WHY THE SYSTEM IS BROKEN. THEY KNOW THIS. THEY’VE KNOWN FOR YEARS. WHY AREN’T THEY DOING ANYTHING? EHRs flag 87% of interactions but 42% are false alarms? That’s not a glitch - that’s negligence. Doctors are lazy. Pharmacies are overworked. And patients? We’re treated like dumb animals who can’t read labels. They’re not fixing this because they don’t want to fix this. They profit off the chaos. You think they care about your kidneys? Nah. They care about your insurance copay. Wake up. This isn’t medicine - it’s a business model built on your suffering.
Look, I get it. You’re all like, ‘Oh my gosh, drug-disease interactions are scary!’ But let’s be real - this is just another way for Big Pharma to scare people into buying more ‘specialized’ meds. You think they actually want you to know about Beers Criteria? Nah. They want you confused, scared, and still buying pills. And don’t even get me started on ‘natural supplements’ being dangerous. Garlic lowers blood pressure? So does not eating salt. Maybe the real problem is we’re all just too damn lazy to eat right and move our butts. Also, why is everyone suddenly so obsessed with kidney numbers? I’ve got a 1998 Toyota Corolla that’s got more maintenance than my doctor’s checklist. Chill out. You’re gonna give yourself a heart attack worrying about your metformin.
It’s appalling. Truly. The fact that 84% of serious interactions in diabetes patients involve kidney issues - and yet, medical education dedicates 4.2 hours to this topic - is a moral failure. You’re not just ‘forgetting’ this - you’re actively endangering lives. And people who say, ‘Just ask your doctor’? That’s not a solution - that’s a cop-out. Doctors are overworked, underpaid, and trained to treat diseases in silos. This isn’t a patient problem - it’s a systemic, institutional failure. If you’re not advocating for mandatory, comprehensive drug-disease interaction training in med school, you’re part of the problem. 🧠🩺
One must acknowledge, with the utmost gravity, that the current paradigm of pharmacological management in the presence of multimorbidity represents a profound epistemological lacuna within contemporary medical science. The reductionist model, predicated upon discrete disease entities, is fundamentally incompatible with the organismic complexity of human physiology. One is compelled to conclude that the prevailing clinical infrastructure - replete with its algorithmic alert fatigue and fragmented specialist paradigms - is not merely inadequate, but epistemologically obsolete. The solution, therefore, lies not in patient vigilance, but in a radical reconceptualization of medical epistemology, grounded in systems biology and interdisciplinary integration. Until then, we are merely rearranging deck chairs on the Titanic.
People need to stop taking supplements. Seriously. St. John’s wort? Ginkgo? Garlic? These are not ‘natural remedies’ - they’re unregulated, untested, dangerous chemicals. And you think your ‘herbal tea’ is harmless? It’s not. You’re playing Russian roulette with your liver. And don’t even get me started on people who think ‘over-the-counter’ means ‘safe.’ It doesn’t. It means ‘not regulated by the FDA.’ You’re not being ‘natural’ - you’re being reckless. And if you’re not getting your creatinine checked yearly, you’re not just irresponsible - you’re selfish. Your health affects everyone around you. Stop being so careless.
Ugh. Another ‘awareness’ post. Great. Now I have to go check my meds AGAIN. Like, I get it. I’m diabetic, I have high BP, I take 7 pills. But you think I don’t already know? I’ve been told this stuff a hundred times. No one’s gonna change. The system’s broken. The doctors don’t care. The pharmacists are busy. And I’m just tired. 😑
As someone from India where people often mix Ayurvedic herbs with Western meds, this hit home. My uncle took ashwagandha with his blood pressure meds - ended up with dangerously low BP. No one told him it could interact. The real issue isn’t just in the U.S. - it’s global. We need simple, clear patient guides in local languages. Not just ‘ask your doctor.’ That’s useless if your doctor doesn’t know either. I’m sharing this with my family. Thank you for writing this.