When patients present with uncontrolled heart rate despite optimal therapy, many clinicians wonder if there’s a safer, more targeted option. Ivabradine offers a unique way to lower heart rate without affecting contractility or blood pressure, making it a valuable tool for chronic heart failure and stable angina. This guide breaks down everything you need to know-from pharmacology to dosing, monitoring, and real‑world pitfalls-so you can prescribe with confidence.
What Is Ivabradine?
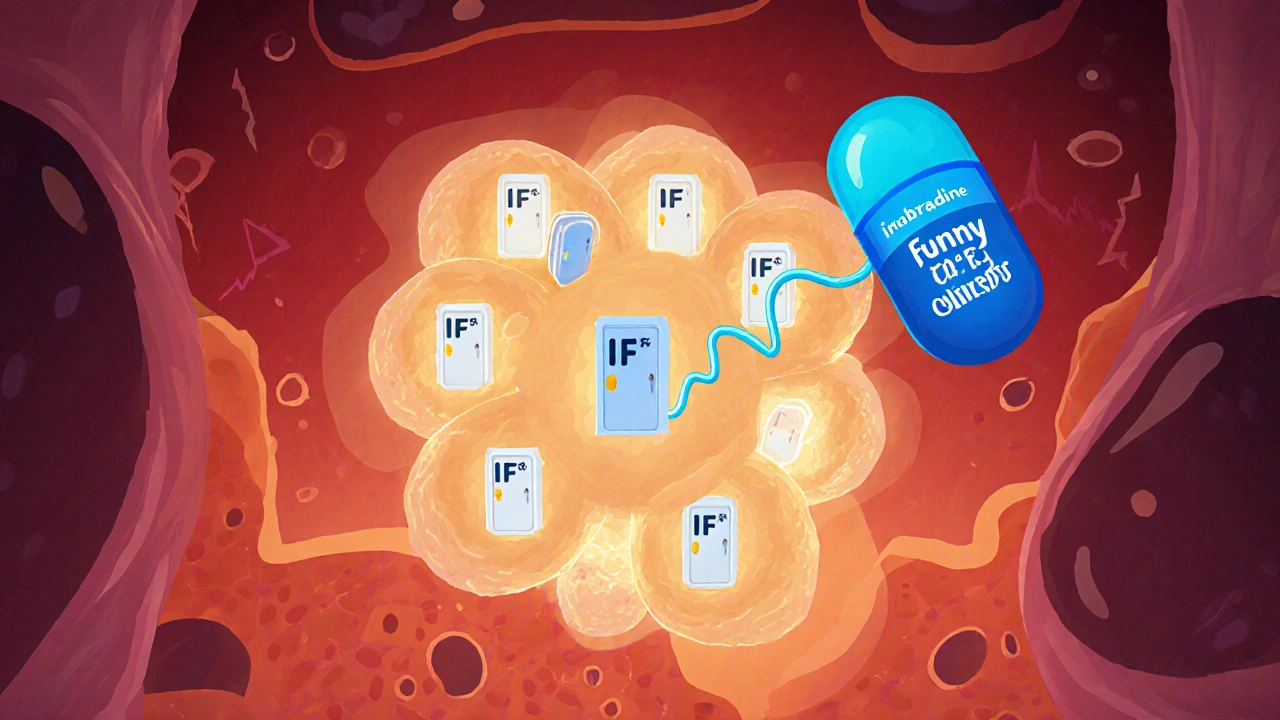
Ivabradine is a selective inhibitor of the funny current (If) in the sinoatrial node. By slowing the spontaneous depolarisation of pacemaker cells, it reduces resting heart rate without altering myocardial contractility or systemic vascular resistance.
Mechanism of Action and Clinical Rationale
Unlike beta‑blockers, which blunt sympathetic drive, ivabradine targets the If channel-a mixed sodium-potassium inward current responsible for the heart’s intrinsic rhythm. The drug binds preferentially to the open state of the channel, a property that gives it use‑dependence: the faster the heart beats, the more channels are open, and the greater the drug effect.
Clinical data show that lowering heart rate to the 50-60 bpm range improves left‑ventricular filling time, reduces myocardial oxygen demand, and can translate into better outcomes for two major indications:
- Chronic heart failure with reduced ejection fraction (HFrEF) where excessive tachycardia accelerates remodeling.
- Stable angina where heart‑rate‑driven oxygen demand is a primary pain driver.
Approved Indications and Guideline Placement
Regulatory approvals differ by region, but most agencies endorse ivabradine for:
- Patients with HFrEF (EF ≤ 35 %) in sinus rhythm, heart rate ≥ 70 bpm, who remain symptomatic despite optimal beta‑blocker therapy or cannot tolerate higher beta‑blocker doses.
- Symptomatic chronic stable angina on maximally tolerated anti‑anginal therapy (beta‑blocker + nitrate ± calcium‑channel blocker) with heart rate ≥ 70 bpm.
Both the 2022 ESC Heart Failure Guidelines and the 2023 AHA/ACC/HFSA guideline list ivabradine as a Class IIa recommendation for HFrEF when heart rate control remains sub‑optimal.
Pharmacokinetics and Drug Interactions
Key pharmacokinetic attributes that affect prescribing:
- Oral bioavailability ~40 %; peak plasma concentrations at 1-2 h post‑dose.
- Extensively metabolised by cytochrome P450 3A4 (CYP3A4). Strong inhibitors (e.g., ketoconazole, clarithromycin) raise ivabradine levels; strong inducers (e.g., rifampicin) lower them.
- Renal clearance accounts for ~15 % of elimination; dose adjustment recommended when eGFR < 30 ml/min/1.73 m².
- Half‑life ~6 h; steady state reached in 2-3 days.
Because ivabradine does not affect the QT interval, it can be combined safely with most anti‑arrhythmic agents, though caution is needed with other bradycardic drugs (e.g., digoxin, non‑DHP calcium‑channel blockers).
Initiation and Titration Protocol
Starting dose and escalation differ by indication:
| Indication | Starting Dose | Target Heart Rate | Maximum Dose |
|---|---|---|---|
| Chronic HFrEF | 5 mg twice daily (BID) | 50-60 bpm | 7.5 mg BID |
| Stable Angina | 5 mg BID | ≤ 60 bpm (symptom relief) | 7.5 mg BID |
Increase to 7.5 mg BID after 2 weeks if heart rate remains > 60 bpm and the patient tolerates the drug. Reduce to 2.5 mg BID if resting heart rate falls below 50 bpm, if symptomatic bradycardia occurs, or if visual disturbances develop.
Monitoring and Follow‑Up
Effective monitoring centres on heart rate, rhythm, and tolerability:
- Baseline ECG to confirm sinus rhythm and QTc < 440 ms.
- Resting heart rate check at 1‑week, 2‑weeks, and then monthly until stable.
- Renal function (eGFR) at baseline and every 3 months for patients with CKD.
- Ask specifically about luminous phenomena (“phosphenes”)-transient flashes of light that resolve after discontinuation.
If bradycardia (< 50 bpm) or symptomatic dizziness persists after dose reduction, consider discontinuation.
Safety Profile and Common Adverse Effects
Ivabradine’s safety record is favourable, but clinicians should watch for:
- Bradycardia: Most common; dose‑dependent.
- Phosphenes: Visual disturbances in up to 10 % of users, usually transient.
- Atrial fibrillation: Slightly increased incidence; routine rhythm checks recommended.
- Hypotension: Rare, because vascular tone is unchanged.
Serious hepatic injury has not been reported, but hepatic impairment can modestly raise plasma concentrations via reduced CYP3A4 activity.
Special Populations
When treating specific groups, adjust expectations:
- Elderly (> 75 years): Start at 2.5 mg BID; frailty increases bradycardia risk.
- Pediatric: Not approved; off‑label use discouraged.
- Pregnancy & lactation: Category B; animal studies show no teratogenicity, but human data are sparse-use only if benefits outweigh risks.
- Renal impairment: Reduce to 2.5 mg BID if eGFR < 30 ml/min/1.73 m².
Clinical Evidence Snapshot
Two landmark trials shape current practice:
- SHIFT (2010): In 6,500 HFrEF patients, ivabradine reduced the composite of cardiovascular death or HF hospitalization by 18 % (HR 0.82, p < 0.001) when added to guideline‑directed therapy.
- ADD‑A‑FIB (2021): In patients with chronic stable angina and heart rate ≥ 70 bpm, ivabradine improved angina frequency by 30 % versus placebo, with no increase in major adverse cardiac events.
Both studies emphasized maintaining sinus rhythm-ivabradine is ineffective in atrial fibrillation because the drug’s target (If channel) is absent in non‑sinus pacemaker tissue.
Practical Tips for the Clinician
- Always confirm sinus rhythm before initiating.
- Document baseline heart rate and aim for 50-60 bpm; avoid overtreatment.
- Educate patients about possible visual flashes; reassure them they are benign and reversible.
- Schedule a follow‑up ECG within 2 weeks of dose escalation.
- When adding ivabradine to a beta‑blocker, ensure the beta‑blocker dose is at least 50 % of the target unless contraindicated.
- Consider a “drug holiday” of 48 hours before elective surgery if bradycardia is a concern.
When Not to Use Ivabradine
Contraindications are straightforward:
- Permanent or persistent atrial fibrillation, atrial flutter, or other non‑sinus rhythms.
- Resting heart rate < 50 bpm before the first dose.
- Severe hypotension (SBP < 90 mmHg).
- Known hypersensitivity to ivabradine or any excipients.
- Concurrent strong CYP3A4 inhibitors without dose adjustment.
Future Directions and Ongoing Research
Investigators are exploring ivabradine in several newer arenas:
- Heart failure with preserved ejection fraction (HFpEF): Early-phase trials suggest heart‑rate reduction may improve exercise capacity, but larger outcome studies are pending.
- Post‑myocardial infarction remodeling: Small studies indicate reduced LV dilatation when ivabradine is started within 48 h of reperfusion.
- Hypertrophic cardiomyopathy: By lowering heart rate, ivabradine may reduce outflow‑tract gradients; a phase‑II trial is currently recruiting.
These investigations could broaden the drug’s label if efficacy and safety are confirmed.
Quick Reference Checklist
- Confirm sinus rhythm and HR ≥ 70 bpm.
- Start 5 mg BID; titrate to 7.5 mg BID if needed.
- Target HR 50-60 bpm.
- Monitor ECG, HR, eGFR, and visual symptoms.
- Avoid strong CYP3A4 inhibitors or adjust dose.
- Discontinue if HR < 50 bpm or symptomatic bradycardia.
Frequently Asked Questions
Can ivabradine replace a beta‑blocker?
No. Ivabradine is an adjunct, not a substitute. Beta‑blockers control both heart rate and sympathetic drive, while ivabradine only slows the SA node. Use it when beta‑blocker dose is maximised or poorly tolerated.
Is ivabradine safe in patients with chronic kidney disease?
Yes, with dose adjustment. For eGFR < 30 ml/min/1.73 m², start at 2.5 mg BID and avoid rapid escalation.
What are phosphenes and how should I counsel patients?
Phosphenes are brief, flickering light spots that some patients see, especially after dose increases. They are harmless and usually disappear after dose reduction or discontinuation. Reassure patients and ask them to report any visual changes promptly.
How does ivabradine interact with digoxin?
Both drugs can lower heart rate, so concurrent use raises the risk of bradycardia. Monitor resting HR closely and consider a lower ivabradine dose if digoxin is required.
Is ivabradine effective in atrial fibrillation?
No. The drug’s target channel is absent in atrial fibrillation; clinical trials have shown no heart‑rate‑lowering benefit in this rhythm.
With a clear understanding of its pharmacology, dosing nuances, and safety considerations, ivabradine can become a reliable ally in managing heart‑rate‑driven cardiovascular disease. Use the checklist, stay vigilant for bradycardia and visual side effects, and align therapy with current guideline recommendations to optimise patient outcomes.

Great overview-Ivabradine truly fills a niche when beta‑blockers aren’t enough.
I always start by confirming sinus rhythm and a resting rate above 70 bpm before the first dose.
Keeping the target heart rate between 50‑60 bpm helps improve ventricular filling without compromising blood pressure.
Remember to schedule a follow‑up ECG after any dose increase to catch bradycardia early.
One practical tip that isn’t in many summaries is to counsel patients about the harmless “phosphenes” they might see; a simple reassurance often prevents unnecessary discontinuation.
If you’re co‑prescribing a CYP3A4 inhibitor, drop the dose to 2.5 mg BID right away.
These small adjustments can make the difference between a smooth titration and a clinic‑room scramble.
Ivabradine can be a game changer for heart rate control, but watch the dosagesage.
The pharmacodynamic profile of ivabradine epitomizes a mechanistic precision that eclipses the nonspecific sympatholytic milieu of conventional beta‑blockade.
By selectively modulating the If current, it attenuates chronotropic stress without perturbing inotropic constancy, thereby preserving myocardial oxygen balance.
Clinical algorithms should integrate this agent as a second‑line chronotropic modifier in sinus‑rhythmic cohorts refractory to optimized β‑adrenergic antagonism.
Take heed of the stochastic variability introduced by concurrent CYP3A4 modulators, which can precipitate supra‑therapeutic plasma concentrations.
Renal insufficiency mandates a dose de‑escalation to mitigate accumulation, especially in eGFR < 30 mL/min/1.73 m².
In sum, ivabradine represents an evidence‑based adjunct that aligns with contemporary guideline directives when employed judiciously.
💥Listen up, folks! Ivabradine is the hidden weapon the American heart‑care system has been ignoring for far too long! 🇺🇸💪 If you’re not using it, you’re basically letting patients suffer unnecessary tachycardia! 😡🚫
Ivabradine works great when you need to drop the heart rate but keep blood pressure stable it’s a solid add‑on for HF patients who can’t tolerate high dose beta blockers just watch the heart rate stay above 50 bpm and check for those funny light flashes they call phosphenes
While the checklist is helpful, one must also consider the ethical implications of prescribing a relatively expensive agent without robust insurance coverage 🤔. Over‑reliance on any single pharmacologic tool risks creating a monoculture of care that may marginalize patients unable to afford the medication. A balanced approach should always incorporate lifestyle modification and patient education as foundational pillars.
Honestly, this guide is just a rehash of what’s already in the product label; nothing groundbreaking here.
Dear colleague, I appreciate your candid assessment, yet I would like to emphasize that the synthesis of guideline recommendations, pharmacokinetic nuances, and practical monitoring strategies presented herein offers a valuable consolidation for clinicians navigating complex therapy decisions. 🌟
When you’re dealing with a patient on digoxin, the additive chronotropic effect of ivabradine can push the HR under 45bpm, which is a red flag for acute brady‑arrhythmia. Make sure to re‑assess the dosing schedule and consider a temporary hold if the patient reports dizziness.
Ivabradine stands out in the therapeutic armamentarium for its unique mechanism of action-targeting the funny current in the sino‑atrial node, thereby offering heart‑rate reduction without compromising myocardial contractility, which is particularly advantageous in patients with heart failure with reduced ejection fraction;
the drug’s pharmacokinetic profile, characterized by an oral bioavailability of approximately 40 percent and metabolism primarily via CYP3A4, necessitates vigilant review of concomitant medications to avoid inadvertent drug‑drug interactions;
clinicians should be mindful that strong CYP3A4 inhibitors, such as ketoconazole, can markedly elevate plasma concentrations, potentially precipitating symptomatic bradycardia or visual disturbances;
conversely, inducers like rifampicin may diminish therapeutic effect, underscoring the importance of dose adjustments based on renal function and hepatic metabolism;
the recommended initiation dose of 5 mg twice daily, with titration to 7.5 mg twice daily after two weeks if the resting heart rate remains above 60 bpm, provides a structured pathway for achieving the target heart rate of 50‑60 bpm;
however, in elderly patients or those with frailty, a starting dose of 2.5 mg twice daily is prudent to mitigate the risk of excessive bradycardia;
routine monitoring should include baseline ECG to confirm sinus rhythm, periodic heart‑rate checks at one‑week and two‑week intervals, and renal function assessments every three months for individuals with chronic kidney disease;
the phenomenon of phosphenes-transient luminous visual sensations-while generally benign, warrants patient education to prevent unnecessary alarm and to differentiate from more serious ophthalmologic events;
published data from the SHIFT trial demonstrated an 18 percent reduction in the composite endpoint of cardiovascular death or heart‑failure hospitalization when ivabradine was added to optimal guideline‑directed therapy, reinforcing its mortality‑benefit potential;
subsequent analyses have highlighted that the benefit is most pronounced in patients with a resting heart rate above 75 bpm, suggesting that baseline tachycardia may serve as a predictive marker for response;
the drug’s safety profile is further bolstered by its neutrality on blood pressure, making it especially suitable for patients who cannot tolerate additional antihypertensive burden;
non‑cardiac adverse events are infrequent, yet clinicians should remain alert for signs of atrial fibrillation, which, although not directly caused by ivabradine, may emerge in the context of altered autonomic balance;
in patients slated for elective surgery, a temporary discontinuation of 48 hours may be advisable to circumvent intra‑operative bradycardia, especially when combined with other negative chronotropes;
finally, ongoing research into ivabradine’s role in heart‑failure with preserved ejection fraction, post‑myocardial infarction remodeling, and hypertrophic cardiomyopathy may expand its indications, provided forthcoming trials confirm efficacy and safety; therefore, staying abreast of emerging evidence is essential for integrating ivabradine appropriately into individualized patient care plans.