Imagine this: you’re a nurse on a late-night shift. A doctor says, "Give the patient the thyroid med." Two vials sit side by side-levoTHYroxine and SYNTHROID. They look identical. The labels are nearly the same. In the rush, you grab the wrong one. The patient gets ten times the dose they need. That’s not a movie plot. That’s a real error that happens more often than you think.
What Are Look-Alike, Sound-Alike (LASA) Medications?
Look-alike, sound-alike (LASA) medications are drugs that are confusing because they look similar on the bottle, sound alike when spoken, or even resemble each other in color and shape. These aren’t just minor mix-ups. They lead to serious harm-overdoses, missed treatments, even death. The World Health Organization calls LASA errors one of the biggest threats to patient safety. In the U.S., about one in four medication errors is caused by drug name confusion. That’s not a small number. That’s a system-wide problem. It’s not just about spelling. It’s about how the name sounds when a doctor says it over a noisy intercom. It’s about two pills that look exactly the same except for a tiny number on the side. It’s about labels that use the same font, color, and layout. All of these things trick the brain into thinking they’re the same thing.How Common Are These Errors?
A 2022 study of hospital records found that drug name confusion caused over 64% of all LASA errors. Packaging confusion made up another 25%. Even the shape and color of pills played a role in over 10% of cases. Some of the most dangerous pairs are within the same drug family. For example:- Simvastatin 10 mg and simvastatin 20 mg
- HydroMorphone and hydroCodone
- Doxorubicin and daunorubicin
- LevoTHYroxine and SYNTHROID
- Vecuronium and Versed
Why Do These Mistakes Keep Happening?
You might think, “Why don’t they just change the names?” The truth is, drug names aren’t chosen with safety as the top priority. They’re chosen for marketing, trademark availability, or to sound scientific. That’s why we end up with names like melphalan and meloxicam-one’s a chemotherapy drug, the other’s a painkiller. They sound almost identical. And in 2024, the Institute for Safe Medication Practices added them to their high-risk list. Even when names are changed, the damage lingers. Hospitals still stock old bottles. Prescribers still say the old names. Pharmacists still reach for the same shelf. The system doesn’t reset when a name changes. And then there’s workload. Nurses and pharmacists are stretched thin. During shift changes, handoffs, or busy hours, attention drops. A quick verbal order like “give the insulin” without specifying type or dose is a recipe for disaster. One nurse on Reddit shared how she almost gave levothyroxine instead of Synthroid during a night shift because the provider just said “thyroid med.”
What’s Being Done to Stop It?
There are tools in place, but they’re not foolproof. Tall Man Lettering is one of the most common fixes. It’s when part of the drug name is capitalized to highlight differences. For example:- HYDROmorphone vs. hYDROcodone
- cisPLATIN vs. caraPLATIN
- LEVOthyroxine vs. SYNTHROID
What Can Be Done Better?
The real solution isn’t just tech or labels. It’s culture. Hospitals need to create their own local LASA lists-not copy-paste from national guidelines. Every facility has different drugs in stock. A name that’s risky in a big city hospital might not even be used in a small clinic. One-size-fits-all lists don’t work. Training matters. Staff need at least 2-4 hours of annual education on LASA risks. In high-risk areas like oncology or critical care, quarterly refreshers are a must. But many places still treat this as a checkbox exercise. And we need to change how we communicate. Say the full name. Spell it out. Don’t say “the insulin.” Say “Lantus 10 units subcutaneous.” Don’t say “the blood thinner.” Say “warfarin 5 mg by mouth.” Voice recognition tech is being tested now. Johns Hopkins is running a $4.7 million study using AI to listen to verbal orders and flag potential LASA mix-ups in real time. Early results show 89% accuracy. That’s promising. But it’s not ready for every hospital yet.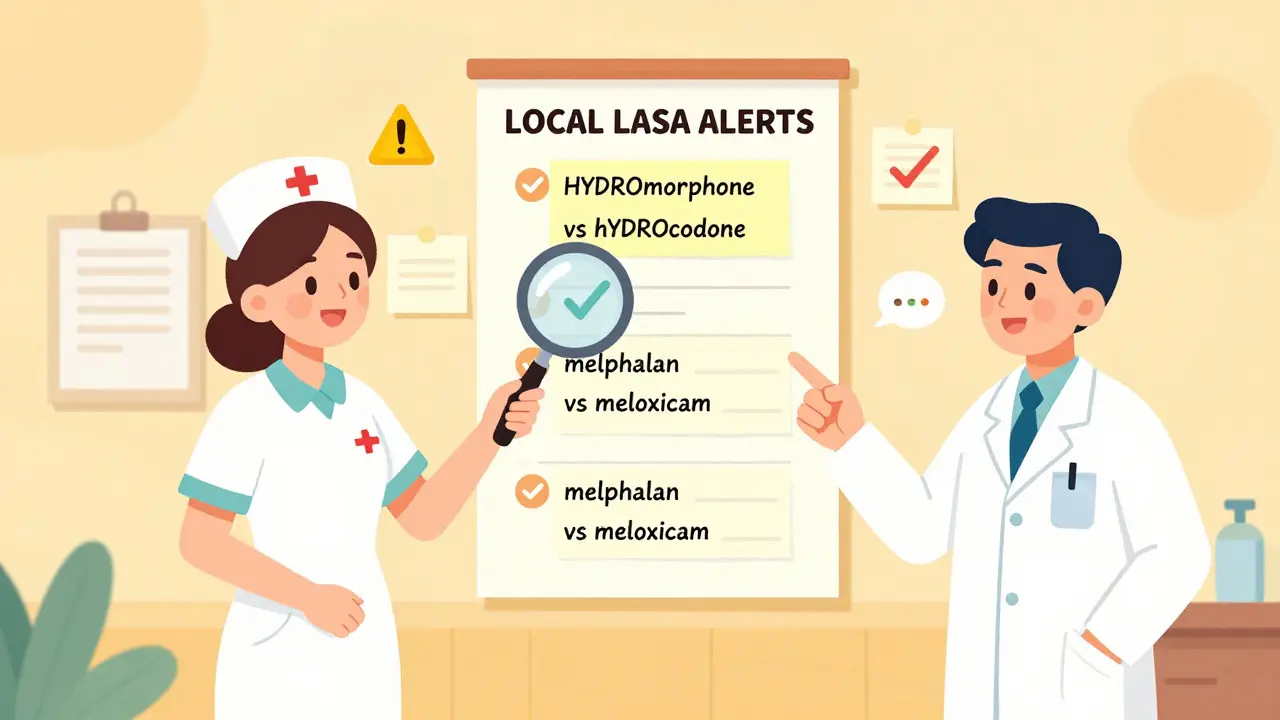
The Bigger Picture
This isn’t just about drugs. It’s about how we design systems that ignore human error instead of planning for it. The World Health Organization says we need a systems-based approach. That means:- Designing drugs with safety in mind from day one
- Using technology that works with the human brain, not against it
- Training staff not just to spot errors, but to prevent them
- Creating a culture where asking for clarification is encouraged, not seen as a sign of weakness
What You Can Do
If you’re a patient, don’t be afraid to ask:- “What’s the full name of this drug?”
- “Is this the same as [other drug I’ve taken]?”
- “Can you spell it for me?”
What are some common look-alike, sound-alike drug pairs?
Common LASA pairs include HYDROmorphone and hYDROcodone, levoTHYroxine and SYNTHROID, doxorubicin and daunorubicin, vecuronium and versed, melphalan and meloxicam, and naltrexone and naloxone. Even small differences in spelling or pronunciation can lead to serious mix-ups, especially in high-stress environments.
How does Tall Man Lettering help prevent errors?
Tall Man Lettering uses capital letters to highlight differences in similar drug names-for example, HYDROmorphone vs. hYDROcodone. It helps the eye catch the distinction quickly. But it only works if staff understand its purpose. If it’s ignored or misunderstood, it becomes a placebo effect with little real impact.
Why aren’t drug names changed to avoid confusion?
Drug names are often chosen for marketing, trademark, or scientific appeal-not safety. Changing names is expensive and disruptive: it requires relabeling, retraining, updating EHRs, and re-educating staff. The FDA now blocks new names that are too similar, but existing names stay in use for years, even when dangerous.
Can electronic health records prevent LASA errors?
Yes, but not always. Systems like Epic and Cerner have built-in alerts for LASA pairs, and studies show they can reduce errors by up to 30%. However, these tools only work if they’re properly configured, regularly updated, and used consistently. Smaller clinics often lack the resources to implement them fully.
Are LASA errors more common in certain settings?
Yes. Hospitals with high volumes of high-alert medications-like ICUs, oncology units, and emergency departments-see the most errors. A 2022 AMA survey found 92% of oncologists reported a LASA near-miss in the past year. Busy shifts, verbal orders, and similar packaging make these areas especially vulnerable.
What should patients do to protect themselves?
Always ask for the full drug name and spelling. Confirm the purpose, dose, and route. If a medication looks different from what you’ve taken before, ask why. Don’t assume it’s the same. Your questions can stop a mistake before it happens.



Let me tell you something that no one in administration wants to admit: this isn't about drug names. It's about profit. Pharma companies deliberately choose names that sound similar because they know nurses are overworked and tired. They count on the mistake. It's not negligence-it's strategy. And when someone dies? They settle quietly. No headlines. No accountability. Just another line in the quarterly report.
bro why are we even talking about this like it's a surprise? nurses get 10 mins to check 30 meds. of course someone grabs the wrong bottle. it's not the nurse's fault. it's the system. fix the system, not the labels.
Oh wow, so now we're blaming Big Pharma AND the EHR vendors? Cute. Meanwhile, the real issue is that 70% of these hospitals still use paper charts from the 90s. You want to fix LASA errors? Start by dumping the legacy junk. Stop buying $200k software that doesn't integrate with your actual workflow. It's not the name-it's the infrastructure.
I’ve been a pharmacist for 22 years. I’ve seen it all. I’ve caught my own mistakes because I took a second to spell it out. I’ve watched coworkers cry after a near-miss. This isn’t about tech or labels. It’s about slowing down. Taking a breath. Saying the full name. It’s not hard. It’s just human. And we forgot how to be human in healthcare.
It is imperative to recognize that the persistence of Look-Alike, Sound-Alike (LASA) medication errors constitutes a systemic failure of governance, oversight, and professional accountability. The absence of mandatory, standardized nomenclature protocols across jurisdictions represents a dereliction of duty by regulatory bodies, compounded by institutional complacency. Furthermore, the reliance on Tall Man Lettering as a primary intervention is empirically inadequate, as it presumes cognitive vigilance in an environment deliberately engineered to erode it. A true systems-based approach requires mandatory pharmacovigilance training, real-time AI-assisted verification, and punitive financial penalties for manufacturers who submit non-compliant nomenclature. Until then, we are not merely failing patients-we are enabling institutionalized harm.
...and yet, somehow, no one mentions that the FDA’s own naming guidelines are written by lobbyists... who have ties to the very companies that produce these drugs... and who... well... you get the point. It’s not a flaw-it’s a feature. The system isn’t broken. It’s working exactly as intended.
tbh i think the real problem is that people dont even read the labels anymore. i work in a pharmacy and half the time people just grab the first bottle that looks right. like dude its a 500mg pill not a 50mg one. how do you miss that???
You think this is about drugs? No. This is about the New World Order. The WHO, FDA, and Big Pharma are all part of the same global cabal. They want you dependent. They want you confused. They want you to take the wrong pill so you get sick again-so they can sell you more. Tall Man Lettering? That’s a distraction. The real solution is to stop trusting any government-approved drug. Go herbal. Go raw. Go off-grid. They don’t want you to know that levothyroxine and Synthroid are the same thing anyway-because if you knew, you’d stop paying for the brand name. And that’s the real crime.