When a child stops growing like they should, parents often blame poor eating habits or late bedtimes. But sometimes, the real culprit is hidden in plain sight-in bread, pasta, and even soy sauce. Celiac disease, an autoimmune condition triggered by gluten, affects about 1 in 133 children in the U.S., and many go undiagnosed for years. Unlike adults who might have bloating or diarrhea, kids with celiac often show up at the doctor’s office simply because they’re not gaining height or weight like their peers. The good news? Once you find out what’s wrong and start a strict gluten-free diet, most children catch up-sometimes completely. But getting there takes more than just cutting out wheat. It takes the right tests, consistent monitoring, and real-world support.
Why Growth Problems Are a Red Flag for Celiac Disease
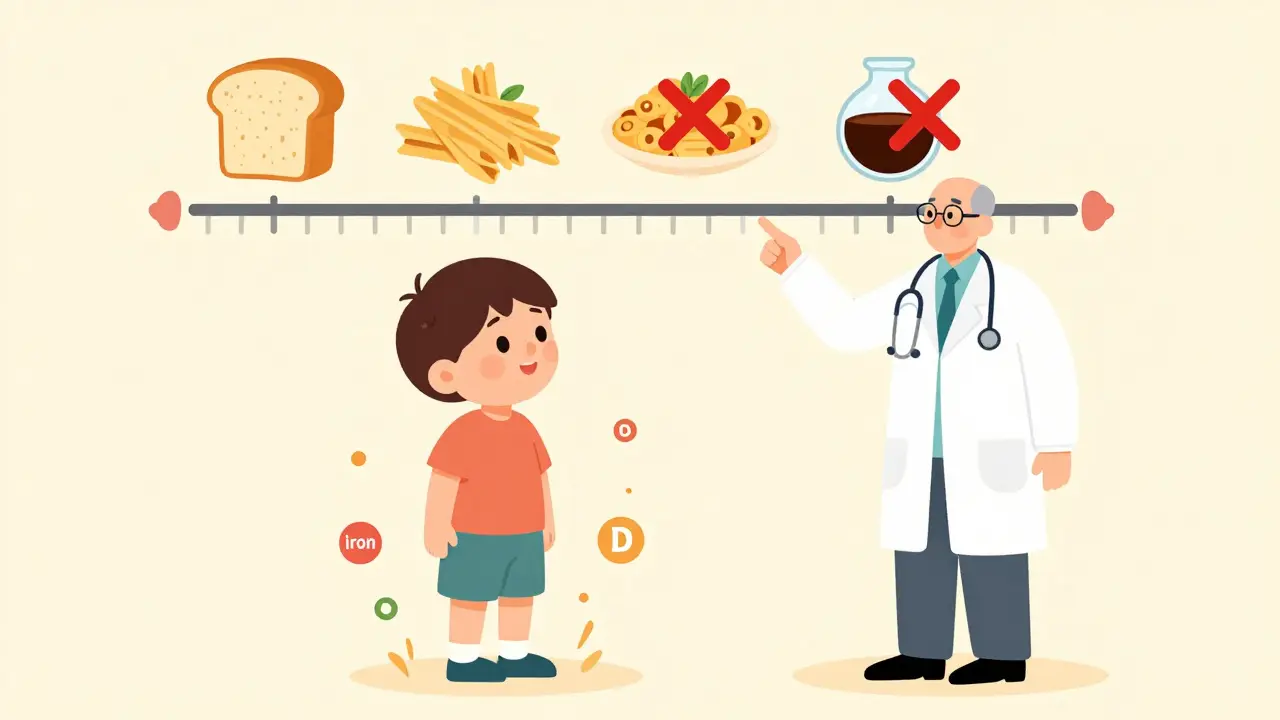
Most parents don’t connect slow growth with an autoimmune disorder. But in children, stunted height is one of the clearest signs of untreated celiac disease. The body’s immune system attacks the lining of the small intestine when gluten is eaten. This damages the finger-like villi that absorb nutrients. Without them, kids miss out on iron, calcium, vitamin D, and protein-all the building blocks for growing taller and stronger.
Studies show that 10 to 40% of children brought in for short stature end up being diagnosed with celiac disease. And it’s not just about being short. Many have delayed bone age-meaning their bones are developing slower than their actual age. One study found that 65 to 75% of kids with growth delays due to celiac had bone age delays of 1.5 to 2.5 years. That’s actually a good sign. It means their body still has time to catch up once gluten is removed.
There are three common growth patterns after starting a gluten-free diet:
- Pattern A: Babies and toddlers diagnosed early bounce back fast. They gain weight and height quickly within the first year.
- Pattern B: Older kids grow slightly faster than normal for their age, but their bone age catches up over time. They end up at their expected adult height.
- Pattern C: Growth velocity stays normal, but bone maturation is delayed. Their growth period stretches out longer than usual, but they still reach their target height.
One 2018 study followed 24 children diagnosed at an average age of 8.3 years. Their height scores improved from -1.77 to -0.95 after three years on a gluten-free diet. That’s a big jump-but it wasn’t complete catch-up. Weight usually rebounds in 6 months. Height? That takes 18 to 24 months. And 85% of kids reach their predicted height by the time they’re done growing.
Testing for Celiac: What Works, What Doesn’t
For years, the only way to confirm celiac was a biopsy-taking a tissue sample from the small intestine. Now, guidelines have changed. The European Society for Pediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN) updated its rules in 2020. If a child has tTG-IgA antibody levels 10 times higher than normal, has the HLA-DQ2 or DQ8 genes, and shows clear symptoms, they might not need a biopsy at all.
Here’s how testing works in practice:
- Start with blood tests: tTG-IgA is the most accurate. It’s 98% sensitive and 95% specific. But you also need to check total IgA levels. About 2 to 3% of people with celiac are IgA deficient, which can give false negatives.
- Check for genes: HLA-DQ2 or DQ8. If they’re negative, celiac is extremely unlikely. If positive, it doesn’t mean they have it-but it means they’re at risk.
- Consider biopsy: Still needed if antibody levels are borderline, or if symptoms don’t match the blood results. Endoscopy can show scalloped folds or mosaic patterns in the intestine. Biopsy results typically show Marsh 3 lesions-total or subtotal villous atrophy.
And don’t skip the basics. Nearly half of newly diagnosed kids have iron deficiency. One in five have iron deficiency anemia. Vitamin D levels are low in 40 to 60%. Folate and B12 are often low too. These aren’t side effects-they’re signs the gut isn’t absorbing anything properly.
Doctors now recommend screening high-risk kids even if they don’t have symptoms. That includes children with type 1 diabetes, Down syndrome, or a first-degree relative with celiac. About 5 to 10% of kids with a family history develop celiac by age 10.
The Gluten-Free Diet: More Than Just No Bread
There’s no medication for celiac. The only treatment is a lifelong gluten-free diet. But “gluten-free” isn’t just about avoiding sandwiches or pizza. Gluten hides in soy sauce, malt flavoring, processed meats, sauces, and even some medications. Cross-contamination is a huge problem-40 to 50% of households accidentally expose their child to gluten through shared toasters, cutting boards, or utensils.
The standard for gluten-free food is 20 parts per million (ppm). That’s tiny. But for a child with celiac, even that small amount can keep the immune system active and block growth.
Here’s what families need to know:
- Safe foods: Fruits, vegetables, meat, fish, eggs, dairy, rice, quinoa, corn, and certified gluten-free oats.
- Hidden dangers: Soy sauce, malt vinegar, modified food starch (unless specified), some spice blends, and even play-dough.
- Label reading: Look for “gluten-free” certification. In the U.S., that means the product has been tested to contain less than 20 ppm.
And the cost? It’s real. Gluten-free products cost 156 to 242% more than regular ones, according to Consumer Reports. For many families, that’s a major burden. One survey found 42% of parents cited cost as their biggest challenge.

Tracking Progress: How You Know the Diet Is Working
Just cutting out gluten isn’t enough. You have to know if it’s helping. Growth is the best indicator.
Here’s what success looks like:
- Weight: Babies gain 15 to 30 grams per day. Older kids gain weight within 6 months.
- Height: A jump of 2 to 4 cm per year above their expected growth rate within the first 6 months.
- Blood tests: tTG-IgA levels should drop to normal within 6 to 12 months. If they don’t, something’s wrong-either hidden gluten or another issue.
- Nutrients: Ferritin (iron storage) should rise above 15 ng/mL. Vitamin D should be above 30 ng/mL. Folate and B12 need to normalize too.
One mom shared that her 7-year-old gained 2.3 kg in the first three months but didn’t start growing taller until 14 months later. That’s normal. Weight comes back fast. Height takes longer.
And here’s the kicker: 20 to 30% of kids show persistent antibody levels even when parents think they’re doing everything right. That’s why quarterly blood tests are non-negotiable. It’s not about being perfect-it’s about catching slip-ups early.
Why Some Kids Don’t Catch Up-And What to Do
Most kids do well. But 5 to 10% don’t reach their full height potential, even with strict diet adherence. That’s not because the diet failed. It’s because something else might be going on.
Doctors look for:
- Growth hormone deficiency
- Other autoimmune conditions (like thyroid disease)
- Chronic inflammation from ongoing gluten exposure
- Severe malnutrition at diagnosis
Children diagnosed before age 5 have a 98% chance of reaching their target height. After age 10? That drops to 85%. The earlier you catch it, the better the outcome.
And if bone age was delayed at diagnosis? That’s a strong predictor of success. One study showed 95% of those kids hit their target height. Only 65% of those with normal bone age did. So if your child’s bones are behind, don’t panic-it’s a sign they still have time.
Adherence Is Hard-Especially for Teens
Young kids usually follow the rules because their parents control what’s on the plate. But teens? That’s where things get messy.
Studies show adolescents have 25 to 35% lower adherence than younger kids. Why? Social pressure. Fear of being different. Wanting to fit in. One 14-year-old told a support group: “I stopped being strict at school. I ate pizza once. Got sick for days. But I didn’t want to be the kid with the weird lunch.”
Parents aren’t the only ones struggling. Schools are a major source of exposure. One survey found 58% of children with celiac had gluten exposure at school. That’s why a 504 plan is essential. It legally requires schools to provide:
- Gluten-free meals
- Dedicated prep areas
- Staff training on cross-contamination
- Permission to carry safe snacks
Support groups help too. Families involved in local celiac chapters see 25 to 30% better adherence. Talking to others who get it makes a difference.
What’s Next? New Treatments on the Horizon
Right now, the only treatment is diet. But researchers are working on alternatives. One drug, larazotide acetate, showed promise in trials-it helps seal the gut lining and reduces symptoms after accidental gluten exposure. Another, Nexvax2, was an immunotherapy vaccine meant to desensitize the immune system. But it failed in Phase 2 trials and was paused in 2022.
Don’t expect a pill anytime soon. Until then, the gluten-free diet remains the gold standard. And for most kids, it works beautifully.
One parent wrote: “My son’s height score went from -2.1 to -0.3 in 18 months. He’s now in the 50th percentile. He’s taller than his older brother.”
That’s the goal. Not perfection. Not instant results. But real, lasting change.
What You Can Do Right Now
If your child is short, slow to gain weight, or has unexplained fatigue, ask for a celiac test. Don’t wait. Don’t assume it’s just a phase. Get the tTG-IgA blood test. Check total IgA. Know their HLA status if possible.
If diagnosed:
- Work with a pediatric dietitian-don’t rely on internet blogs.
- Test nutrient levels every 3 to 6 months.
- Keep a food and symptom journal.
- Get a 504 plan if your child is in school.
- Join a support group. You’re not alone.
Celiac disease doesn’t have to limit a child’s future. With the right diagnosis and support, most grow up healthy, tall, and strong. The key is catching it early-and sticking with it.
Can celiac disease be outgrown?
No. Celiac disease is a lifelong autoimmune condition. The immune system will always react to gluten. There is no cure, and stopping the gluten-free diet-even for a short time-can cause intestinal damage and increase long-term health risks, including lymphoma. Strict, lifelong adherence is the only treatment.
Is a gluten-free diet healthy for a child without celiac?
Not necessarily. Many gluten-free products are lower in fiber, iron, and B vitamins, and higher in sugar and fat. Unless a child has celiac disease, non-celiac gluten sensitivity, or a wheat allergy, there’s no proven benefit to avoiding gluten. In fact, unnecessarily restricting grains can lead to nutritional gaps in growing children.
How long does it take for a child to start feeling better after going gluten-free?
Many children feel better within days to weeks-less bloating, more energy, fewer stomach aches. But physical healing takes longer. Intestinal villi begin to regrow in weeks, but full recovery can take 6 to 18 months. Growth improvements follow, with weight bouncing back faster than height.
Can a child with celiac disease eat oats?
Pure, uncontaminated oats are generally safe for most children with celiac disease. But most oats are processed in facilities that also handle wheat, barley, or rye. Only certified gluten-free oats should be used. Start with small amounts and monitor for symptoms. Always consult your dietitian before adding oats to the diet.
What if my child’s tTG-IgA levels stay high after 12 months on a gluten-free diet?
This means gluten is still being consumed-either knowingly or accidentally. Common causes include cross-contamination at home or school, hidden gluten in sauces or medications, or eating “gluten-free” products that aren’t truly safe. A dietitian review, home audit, and school check are essential. In rare cases, it may signal another condition like refractory celiac disease, which requires specialist evaluation.
Does celiac disease affect puberty?
Most children with celiac disease start puberty at the normal age. But at diagnosis, 15 to 20% may have delayed puberty due to malnutrition. Once on a gluten-free diet, puberty usually begins normally within 6 to 12 months. Persistent delay after dietary adherence should be evaluated by a pediatric endocrinologist.
Are there any long-term risks if celiac disease isn’t treated?
Yes. Untreated celiac disease increases the risk of osteoporosis, infertility, neurological disorders, and certain cancers-especially lymphoma. Studies show non-adherence raises lymphoma risk by 2 to 3 times. It also leads to permanent growth loss in about 15% of cases. Early diagnosis and strict diet adherence eliminate these risks.
Children with celiac disease don’t need to be defined by their condition. With the right support, they can thrive-growing taller, stronger, and healthier than ever before.
My daughter was diagnosed at 6 after years of being in the 5th percentile for height. We thought she was just a late bloomer. Once we went gluten-free, she gained 12 pounds in 4 months and grew 3 inches in a year. It’s not magic-it’s biology. Don’t wait for a crisis. Get tested.
Also, certified gluten-free oats changed our lives. We used to think they were unsafe, but our dietitian said to start small. Now she eats them every morning. Just read labels. Always.
It is imperative to underscore that the diagnostic criteria for pediatric celiac disease, as delineated by the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN), have undergone significant revision since 2020. Specifically, the threshold for tTG-IgA titers exceeding tenfold the upper limit of normal, in conjunction with the presence of HLA-DQ2 or DQ8 haplotypes and corroborative clinical manifestations, now permits the omission of endoscopic biopsy in select populations. This paradigm shift, while evidence-based, necessitates rigorous adherence to protocol to avoid false positives or misdiagnosis.
Furthermore, the assertion that 85% of children achieve predicted adult height is statistically valid, yet it obscures critical heterogeneity in growth trajectories. The variance between Pattern A, B, and C is not merely academic-it dictates clinical monitoring frequency, nutritional supplementation strategy, and psychological support intensity. Parents must be educated accordingly.
People act like gluten is the devil but the real problem is how we eat now. Processed food, sugar, chemicals. Celiac is just the body screaming because everything’s poisoned. Cut out the junk, not just bread. Kids grow better when they eat real food-meat, eggs, veggies. Gluten-free junk food is still junk. You’re not fixing the problem by swapping a wheat bun for a gluten-free one made with rice starch and high fructose corn syrup.
Also why are we so obsessed with height? Kids aren’t widgets. Let them grow at their own pace.
Thank you for this comprehensive overview. As a pediatric dietitian, I see this daily. The most common mistake? Assuming ‘gluten-free’ on the label means safe. It doesn’t. Cross-contamination is the silent killer-especially in households where one member eats gluten. A shared toaster can expose a child to 100x the safe limit.
Also, many parents don’t realize that vitamin D deficiency can persist even after months on a gluten-free diet. I recommend 1,000–2,000 IU daily for children, depending on weight and baseline levels. And always check ferritin-not just hemoglobin. Iron stores take longer to rebuild.
Lastly, support groups are non-negotiable. Isolation is the biggest barrier to adherence. Connect. Share. Survive together.
in india we dont have much awareness. my cousin’s kid was diagnosed at 12 because he was super thin and always tired. family thought he had worms. we went to a private doc who asked for blood test. turns out he had celiac. now he eats rice, dal, curd, and fruits. no bread, no noodles. he’s taller now. but the gluten-free stuff here is expensive and fake. most brands just say ‘gluten-free’ but it’s not tested. you gotta trust the brand or make your own.
also, why do people think gluten is bad for everyone? my mom still says ‘if you eat gluten-free you’ll be healthy’-no, only if you have celiac. normal kids need whole grains. they need the fiber.
I’m a mom of a 10-year-old with celiac and I just want to say-you’re not alone. The grocery bills are insane. The school battles are real. The fear of accidental exposure? Constant. But seeing my kid run around like a normal kid now? Worth every penny, every tear, every label I’ve read at 2 a.m.
Also, we started a ‘gluten-free snack box’ for school. I put it in her backpack with a note: ‘My snack, not yours.’ No drama. No shame. Just safety. Kids get it. They just want to fit in. Give them the tools.
THIS IS WHY AMERICA IS FALLING APART. Parents let their kids eat garbage, then cry when they get sick. You think gluten-free cookies are a solution? NO. You think letting your teen eat pizza at school is okay? NO. You think skipping a blood test because it’s ‘too expensive’ is acceptable? NO.
My daughter had to go to the ER because her teacher gave her a ‘gluten-free’ cupcake that had wheat flour in it. That’s not an accident-that’s negligence. Schools need to be held accountable. And parents need to stop being lazy. This isn’t a trend. It’s a life-or-death condition. Stop making it about your convenience.
so if a kid has normal bone age but still doesn't catch up in height after 2 years gluten-free what does that mean
my son's bone age was normal at diagnosis but he's only grown 1.5 cm in 2 years. tTG is normal now. iron and vit d are good. what else could it be
It is a moral failing, a societal collapse, and a direct consequence of modern parental apathy that we allow our children to be exposed to gluten-containing products in schools, cafeterias, and even in the homes of relatives who refuse to take this condition seriously. The fact that 58% of children with celiac experience exposure at school is not an oversight-it is a systemic betrayal. The government funds school lunches, yet fails to mandate truly gluten-free preparation protocols. This is not negligence-it is complicity.
And let us not forget the economic exploitation: corporations profit from the desperation of parents by charging 242% more for products that are, in many cases, no more nutritious than their gluten-laden counterparts. This is capitalism at its most predatory. The only cure is not diet-it is revolution.
Furthermore, the normalization of ‘gluten-free’ as a lifestyle choice for the non-diagnosed is a dangerous distraction. It dilutes the urgency of the condition, undermines the legitimacy of those who suffer, and encourages false self-diagnosis. You do not have ‘sensitivity.’ You have a preference. There is a difference.
Ugh I'm so tired of this gluten stuff. Everyone's got some autoimmune thing now. My cousin's kid had celiac and she was just a picky eater. They made her eat weird rice cakes and she cried for pizza. Big deal.
And why do we care if a kid's tall? My brother was short his whole life. He's a damn engineer now. Who cares about height? You think the kid's gonna get a job because he's in the 50th percentile? Nah. He'll be fine.
Also, why are we spending all this money on tests? Just give 'em vitamins and stop being so paranoid. This country's gone soft.
Gluten-free is a scam. Rich people buy expensive food and feel superior. Poor people can't afford it so their kids suffer. The real problem is inequality. Not gluten.
Also why do you think science cares about your kid's height? It's just numbers. Let nature take its course. Stop overmedicalizing childhood.