Most people think hearing aids go in your ear. But what if the solution doesn’t need to go in your ear at all? Bone-conduction hearing aids work by sending sound straight through your skull bone to your inner ear, skipping the outer and middle ear entirely. This isn’t science fiction-it’s a proven, FDA-approved option for people who can’t use traditional hearing aids because of chronic ear infections, birth defects, or single-sided deafness.
How Bone-Conduction Hearing Aids Actually Work
Sound normally travels through the air, into your ear canal, vibrates your eardrum, and then moves three tiny bones before reaching the cochlea. But if your ear canal is blocked, your eardrum is damaged, or those bones don’t work right, that path is broken. Bone-conduction devices bypass all that. They turn sound into vibrations and send them through the bone behind your ear-right to the cochlea. It’s like tapping on your skull and hearing the sound inside your head. This method works because your bones naturally conduct sound. You’ve probably felt this yourself when you chew loudly or hum-you hear it differently than when someone else does it.
The science behind this goes back to the 1950s, when Swedish surgeon Per-Ingvar Brånemark discovered titanium could fuse with bone. That breakthrough led to the first Bone-Anchored Hearing Aid (BAHA) in 1977. Today, the technology is refined, reliable, and used by tens of thousands worldwide.
Who Benefits Most From Bone-Conduction Devices
These aren’t for everyone. But for certain types of hearing loss, they’re the best-or only-option.
- Conductive hearing loss: When sound can’t move through the outer or middle ear due to blockages, infections, or malformed ear structures. People with chronic ear infections often can’t wear traditional hearing aids because moisture gets trapped and causes more problems. Bone-conduction devices avoid the ear canal completely.
- Mixed hearing loss: A combination of conductive and sensorineural loss. If the conductive part is the main barrier, bone conduction helps.
- Single-sided deafness (SSD): This is where one ear has normal hearing and the other is completely deaf. Traditional hearing aids can’t help here because they amplify sound on the bad side. Bone-conduction devices pick up sound from the deaf side and send it to the good ear. Many users report hearing birds, traffic, or conversations from their deaf side for the first time in years.
Studies show speech understanding in noisy places improves by 20-35% for SSD users with bone-conduction devices. For people with congenital aural atresia (a birth defect where the ear canal never formed), success rates are 85-90%.
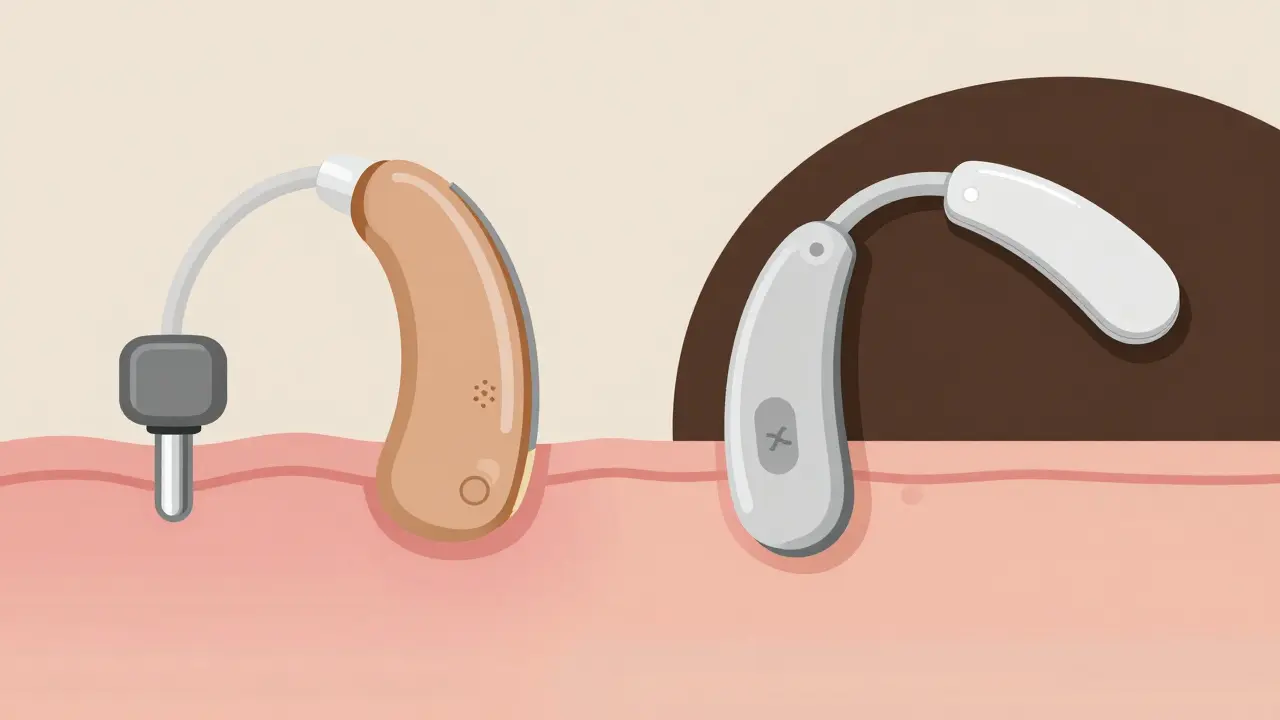
Percutaneous vs. Transcutaneous: Two Different Systems
There are two main types of bone-conduction devices, and they’re very different in how they’re worn.
Percutaneous systems (like Cochlear’s BAHA Connect and Oticon’s Ponto) require a small titanium implant fused into the skull bone. After 3-6 months of healing, an external abutment sticks out through the skin. The sound processor snaps onto it. These are powerful-up to 50 dB of gain-and offer the clearest sound transmission because there’s no skin or tissue between the device and the bone. But they come with a trade-off: skin issues. About 15-30% of users develop irritation, infection, or overgrowth around the abutment. Daily cleaning with 70% isopropyl alcohol is mandatory.
Transcutaneous systems (like MED-EL’s Bonebridge and Cochlear’s BAHA Attract) don’t break the skin. Instead, a magnet inside the skull holds the external processor in place. The sound passes through the skin via magnetic coupling. These are more discreet-no visible post-and have fewer skin complications. But because sound has to travel through skin and tissue, they lose about 10-15 dB of power. That makes them less ideal for people with severe hearing loss. Still, satisfaction rates are higher: 92% of Bonebridge users prefer the invisible design over visible abutments.
Cost, Surgery, and Recovery
These aren’t over-the-counter devices. You need surgery. It’s a minor outpatient procedure-30 to 60 minutes under local anesthesia. Most people go home the same day and return to normal activities within 48 hours.
For percutaneous systems, you wait 3-4 months for the implant to fuse with bone before the processor is turned on. Transcutaneous systems can be activated right after surgery. But even then, your brain needs time to adjust. Sound through bone feels different-quieter, muffled at first. Most users need 2-4 weeks of auditory training to fully adapt.
Cost is a big factor. Implantable bone-conduction devices range from $4,000 to $7,000 per ear. That’s more than double the price of premium air-conduction hearing aids ($1,500-$3,500). Insurance coverage varies. In the U.S., Medicare and many private insurers cover them if you meet medical criteria-like documented conductive loss or SSD with failed trial of CROS aids. In Sweden, where the technology started, 1.2% of hearing-impaired people use bone-conduction devices. In the U.S., it’s only 0.4%-meaning many who could benefit still don’t know about them.
Real User Experiences
Reddit threads and patient surveys paint a clear picture. On r/Hearing, 78% of recent users with single-sided deafness say their quality of life improved dramatically. One user wrote: "I heard a bird chirp from my deaf side for the first time in 15 years. I cried." Another said: "No more earwax buildup. No more itchy, sore ears. Finally, I can wear headphones without pain." But it’s not perfect. About 23% of users report problems with MRI scans. Most implants are MRI-unsafe above 1.5 Tesla, meaning you’d need surgery to remove the device before a scan. That’s a serious concern for older adults or those with chronic conditions requiring frequent imaging.
And skin reactions? Still a problem. Cochlear’s 2022 registry found 28% of BAHA Connect users had skin issues severe enough to need medical attention. Eight percent needed revision surgery. Transcutaneous systems cut that risk significantly.

What’s New in 2026
The field is evolving fast. In 2023, Cochlear launched the BAHA 6 Max with Bluetooth 5.3, 30-hour battery life, and direct streaming from phones. MED-EL is preparing Bonebridge 3, set to launch in early 2024, with AI-powered noise reduction that adapts in real time.
The biggest shift? Transcutaneous systems now make up 63% of new implants-up from 41% in 2019. Why? Fewer complications. Better cosmetics. More confidence.
And the future? Fully implantable devices. No external processor at all. Sonova is in Phase III trials for one, with FDA submission expected by late 2024. If approved, this could be the next big leap-like going from hearing aids to cochlear implants, but without the need for a visible device.
When Bone-Conduction Doesn’t Work
It’s important to know the limits. These devices won’t help if your cochlea is severely damaged. If your sensorineural hearing loss is worse than 45-55 dB, bone conduction won’t be enough. The device can only deliver sound to a working inner ear. No amount of vibration will fix a dead cochlea.
Also, if you have very thick skin behind the ear (more than 5 mm), transcutaneous systems may not transmit enough power. Your audiologist will test this with a trial device before surgery.
How to Decide If It’s Right for You
If you’ve been told you can’t use regular hearing aids because of ear infections, malformed ears, or single-sided deafness, ask your audiologist about bone conduction. Here’s what to do:
- Get a full hearing test, including bone-conduction thresholds.
- Try a non-surgical bone-conduction trial device (like the BAHA SoundArc or Ponto Softband). Wear it for 2-4 weeks.
- Ask about your specific anatomy: skin thickness, bone density, history of infections.
- Discuss MRI needs and long-term maintenance.
- Compare costs and insurance coverage.
Don’t assume you’re stuck with silence or poor sound quality. Bone-conduction hearing aids have helped people who thought they had no options. They’re not for everyone-but for the right person, they’re life-changing.
Can bone-conduction hearing aids help with tinnitus?
Bone-conduction devices don’t cure tinnitus, but they can reduce its perception in people with single-sided deafness. By restoring sound input to the deaf side, the brain has less reason to generate phantom noise. Many users report tinnitus becoming less noticeable after using a bone-conduction device, especially if the tinnitus is in the deaf ear.
Are bone-conduction hearing aids visible?
It depends. Percutaneous systems have a small metal post sticking out behind the ear-visible if you look closely. Transcutaneous systems have no external post; the processor sits flat against the skin and is hidden under hair. Most users find them discreet, especially with longer hair or when worn under hats or headbands.
Can I swim or shower with a bone-conduction hearing aid?
The external processor is water-resistant but not waterproof. You can wear it in light rain or sweat, but you must remove it before swimming, showering, or using a sauna. Some users use protective covers or cases. The implanted part (titanium or magnet) is safe underwater-only the external part needs protection.
Do bone-conduction devices work with phones and TVs?
Yes. Newer models like the BAHA 6 Max and Ponto 5 SuperPower have Bluetooth 5.3 and can stream calls, music, and TV audio directly. You can also use a remote microphone or TV streamer. This makes them far more versatile than older models.
Is there a non-surgical option?
Yes. Softband or headband systems (like the Ponto Softband or BAHA SoundArc) hold the processor against the skull without surgery. These are great for testing before committing to implants, or for children under five who aren’t candidates for surgery. They’re less effective than implanted systems but offer a risk-free trial.

OMG I just tried the Ponto Softband for a week and I swear I heard my cat purr from my deaf side for the first time since I was 12. I cried in the grocery store. Like… actually cried. No joke. This thing is magic.