When your generic pill comes from overseas, how does the FDA make sure it’s safe?
You take a generic medication every day-maybe for blood pressure, cholesterol, or diabetes. You assume it works just like the brand-name version. But here’s the thing: 80% of the active ingredients in those pills, and 40% of the finished drugs, are made in factories overseas, mostly in India and China. The FDA doesn’t just trust those factories. They inspect them. But until recently, the rules weren’t the same for factories in the U.S. versus factories abroad.
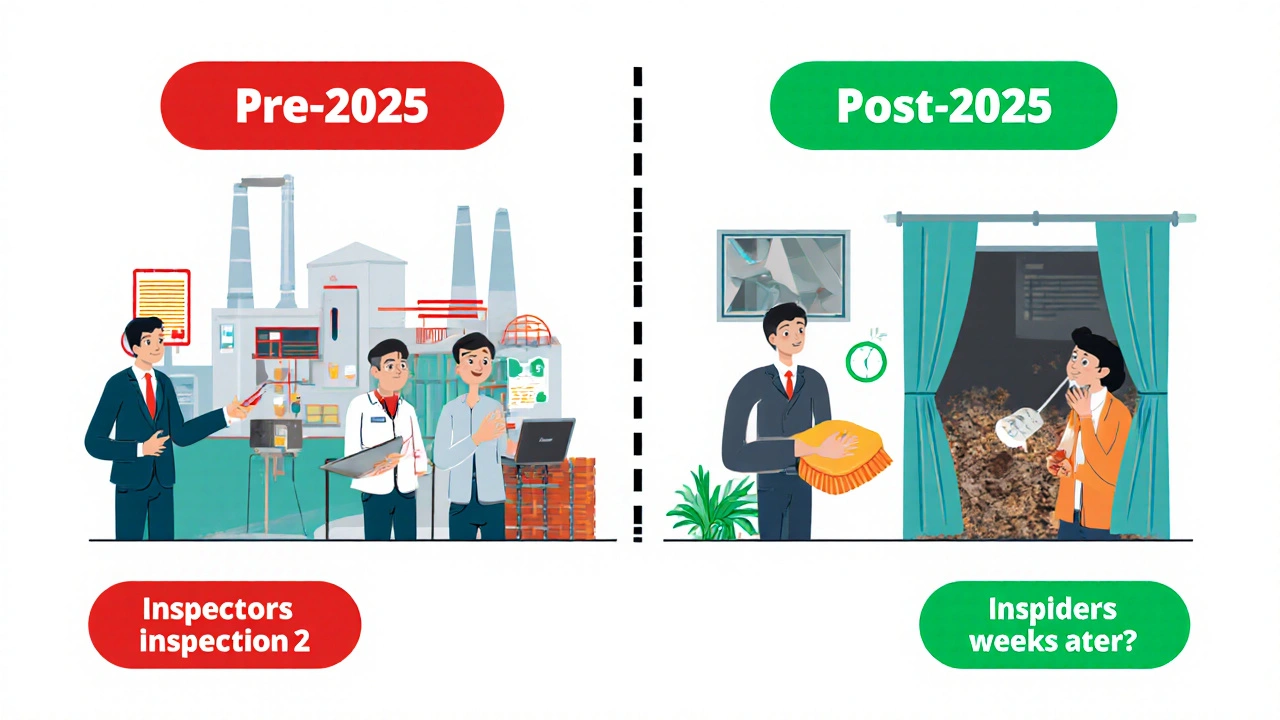
For years, U.S. facilities got surprise inspections. No warning. No time to clean up. Foreign factories? They got notice-sometimes 8 to 12 weeks ahead. That meant they could fix problems just before inspectors showed up. It wasn’t fair. And it wasn’t safe.
What the FDA actually checks during inspections
The FDA doesn’t care where a drug is made. They care if it meets Current Good Manufacturing Practices (CGMP). That’s the rulebook for making safe, effective medicine. It covers everything: how workers wash their hands, how machines are cleaned, how tests are recorded, and whether data gets altered.
During an inspection, FDA inspectors look at:
- Training records for staff-do they know how to prevent contamination?
- Equipment logs-when was the last time the mixer was calibrated?
- Testing results-do the numbers match what’s on the paperwork?
- Raw material storage-is there mold growing near the ingredients?
- Documentation-was a test skipped and then backdated?
They use Form 483 to list problems. If something’s seriously wrong, they issue a warning letter. If the company ignores it, the FDA can block all shipments from that factory. That’s called an import alert.
The double standard that changed in 2025
In 2024, the FDA found 45% of foreign facilities had serious violations-things like falsified test results or poor contamination control. At U.S. facilities? Only 20% had those same issues. Why? Because foreign inspections were predictable.
On May 6, 2025, the FDA announced a major shift. No more advance notice for foreign factories. Unannounced inspections are now the rule, not the exception. By mid-2026, at least half of all foreign inspections will be surprise visits. That’s up from just 15% before.
FDA Commissioner Marty Makary said it plainly: “We’re not going to let manufacturers hide bad practices behind a calendar.”
This change didn’t come out of nowhere. In 2024, ProPublica exposed how Sun Pharma’s facility in India was banned from exporting drugs in 2021-but four of its medicines still made it into U.S. pharmacies. That kind of gap can’t be ignored.
Why India and China dominate generic drug production
India makes about 40% of the active ingredients used in U.S. generic drugs. China supplies another 13%. Together, they produce the bulk of pills Americans take every day.
Why? Cost. Labor. Scale. These countries have factories built for volume, with lower overhead than U.S. plants. But volume doesn’t equal quality. And that’s where oversight breaks down.
Before 2025, the FDA had only about 3,000 inspectors covering more than 90 countries. Meanwhile, they did 12,000 inspections in the U.S. every year. That’s a ratio of 4:1. The math didn’t add up. And neither did the safety.
What foreign manufacturers must do now
If you run a generic drug factory in Pune or Shanghai, the rules just got tougher. You can’t just polish the floor before an inspection. You need to be ready every day.
Here’s what experts recommend:
- Run mock inspections every quarter. Pretend the FDA is coming tomorrow.
- Train staff daily on documentation. No backdating. No deleting data.
- Keep real-time digital logs. Paper records are too easy to tamper with.
- Fix contamination risks before they’re found. That means air filters, gowning procedures, and cleanroom protocols.
- Designate a compliance officer. Someone whose job is to watch the system, not just run it.
A survey by the Parenteral Drug Association found that 68% of foreign manufacturers expect compliance costs to rise 15-25%. Smaller companies are especially vulnerable. Some may not survive. But the ones that adapt? They’ll keep selling to the U.S. market.
The quiet push for a U.S.-based quality gatekeeper
Right now, a foreign factory can ship drugs to the U.S. with no one in America legally responsible for checking each batch. The FDA inspects the factory-but not the shipment.
Some experts, like Dr. Ameet Sarpatwari from Brookings Institution, say that’s a flaw. He suggests adopting a model used in Europe: every batch must be signed off by a Qualified Person-a certified professional who lives in the importing country and takes legal responsibility for the drug’s quality.
It’s not just about safety. It’s about accountability. If a batch causes harm, someone in the U.S. should be answerable-not just a factory manager in another country.
Sens. Kirsten Gillibrand and Tim Scott raised this issue in April 2025, asking the FDA to investigate whether safety concerns were being overridden by internal pressure. Their letter cited cases where the Center for Drug Evaluation and Research approved drugs even after inspectors flagged serious violations.

What’s next? More inspectors, more pressure
The FDA is hiring 200 new foreign inspection specialists by 2026. That’s a 40% increase in inspection capacity. They’re also sharing inspection data with regulators in Europe, Japan, and Australia through mutual recognition agreements.
President Trump’s Executive Order 14135, signed in May 2025, demands that the FDA eliminate the inspection gap within 18 months. That means by late 2026, foreign factories will be held to the same standard as U.S. ones-no exceptions.
Will this cause drug shortages? Maybe in the short term. Evaluate Pharma predicts a 15-20% disruption in generic drug supply as factories scramble to comply. But long-term? It means safer medicine.
What this means for you
You don’t need to know how a tablet is made. But you should know that the system is changing. The FDA is no longer playing catch-up. They’re catching bad actors before they ship.
If your generic pill tastes different, looks different, or seems less effective, report it. The FDA tracks adverse events. One report could lead to an inspection.
And if you’re a patient relying on low-cost generics-this is good news. Stronger oversight means fewer contaminated, under-dosed, or fake drugs entering the U.S. supply chain. It’s not perfect. But it’s moving in the right direction.
How to stay informed
Check the FDA’s website for inspection reports. They publish warning letters and import alerts publicly. If a drugmaker you trust gets a warning, look for alternatives. Your pharmacist can help.
Don’t assume “made in the U.S.” is safer. Many U.S.-branded generics are made overseas too. The label doesn’t tell you where the active ingredient came from. Only the FDA does.
The bottom line: The system is getting tougher. And that’s how it should be.
Are generic drugs made overseas less safe than those made in the U.S.?
Not inherently. The same FDA standards apply to every factory, no matter where it is. But until 2025, foreign factories had a big advantage: advance notice before inspections. That allowed them to hide problems. Now, with unannounced inspections, the playing field is leveling. Factories that cut corners are getting caught more often.
How often does the FDA inspect foreign drug factories?
Before 2025, the FDA inspected about 3,000 foreign facilities each year-far fewer than the 12,000 domestic ones. Now, the goal is to conduct unannounced inspections at 50% of all foreign sites by mid-2026. The FDA is hiring 200 new inspectors to make that happen.
What happens if a foreign factory fails an FDA inspection?
The FDA issues a Form 483 listing violations. If the problems aren’t fixed, they send a warning letter. If the company ignores it, the FDA can place an import alert-blocking all shipments from that facility. In severe cases, the facility may be banned from exporting to the U.S. permanently.
Can I tell if my generic drug was made overseas?
Not from the label. The FDA doesn’t require manufacturers to list where the active ingredient is made. Even if the pill is packaged in the U.S., the key chemical might come from India or China. The only way to know is to check the FDA’s public inspection database or contact the manufacturer directly.
Why does the FDA allow drugs from factories with past violations to still be sold?
Sometimes, the FDA allows a facility to resume exports after it fixes the problems and proves compliance. But there have been cases where violations were downplayed. In 2024, ProPublica found that Sun Pharma’s facility, banned in 2021, still shipped four drugs to the U.S. after the ban. That’s why lawmakers are pushing for stronger oversight and U.S.-based accountability.
Will this increase the cost of generic drugs?
Yes, in the short term. Smaller foreign manufacturers say compliance costs could rise 15-25%. Some may shut down, reducing competition. But long-term, better quality means fewer recalls, fewer lawsuits, and fewer hospitalizations from bad drugs-which saves the healthcare system money.
Is the FDA working with other countries to improve oversight?
Yes. The FDA shares inspection reports and training with regulators in the European Union, Japan, Australia, and Canada through mutual recognition agreements. This helps avoid duplicate inspections and builds global standards. But the U.S. still lags behind the EU’s requirement for a local Qualified Person to certify each batch before release.



sooo… let me get this straight-80% of the active stuff in my blood pressure pills is made in a factory where the inspectors get a *calendar invite*? like, ‘hey, don’t forget to scrub the floors on tuesday, we’re coming!’? 🤦♀️
and now they’re just gonna show up unannounced? finally. i’ve been taking these generics for 12 years and never once thought about whether the guy who packed my tablet washed his hands after using the bathroom. now i’m paranoid. and honestly? good.
also-why does the label say ‘manufactured in the usa’ when the active ingredient came from a village in telangana? that’s not transparency. that’s a magic trick.
OMG YES. I just Googled my lisinopril and found out it’s from a plant in Hyderabad that got a warning letter in 2022. 😱
imagine if your phone charger was made in a factory that got caught faking safety tests… but you still used it. that’s literally what we’re doing with our meds. 🙈💊
china and india are running a global pharmacy scam and the fda was asleep at the wheel. now they’re finally waking up? good. but it’s too little, too late. we need to ban foreign drug manufacturing entirely. every pill made in america. period.
if you can’t make it here, you don’t deserve to sell it here. this isn’t globalism-it’s national security. 🇺🇸✊
hey, i know this is heavy stuff, but let’s celebrate the win! 🎉
unannounced inspections? 200 new inspectors? mutual agreements with eu and australia? this is HUGE. the system’s finally catching up. yeah, prices might spike short-term, but imagine fewer people getting sick from fake meds. that’s worth it.
to all the small manufacturers out there: you got this. get compliant, stay honest, and you’ll survive. we’re rooting for you! 💪
as someone who’s worked in a cGMP-certified facility in Hyderabad for 14 years, i can tell you-this change was inevitable. the old system was a joke. factories would ‘clean’ for inspections like it was a wedding day, then go right back to cutting corners. the real issue isn’t the location-it’s the culture of compliance.
we used to backdate records because the QA manager was afraid of losing his job if he reported delays. now? if you falsify data, you’re looking at jail time. that’s the real shift.
the cost increase? yes. but it’s not just about money-it’s about dignity. we’re not just making pills-we’re making people’s lives. and dignity doesn’t come cheap. but it’s non-negotiable.
also, the qualified person model? brilliant. if a batch kills someone in the US, the liability should sit with someone who lives under US law. not some distant plant manager who doesn’t even speak english.
the fda’s doing the right thing. now let’s fund them properly. 3,000 inspectors for 90 countries? that’s like sending one cop to patrol all of california. we need more eyes. more teeth. more accountability.
and yes, we’re scared. but we’re also proud. because now, the world sees us as partners-not loopholes.
you know what’s wild? i used to think generics were just ‘cheap versions.’ now i realize they’re the only reason i can afford my diabetes meds. and if they’re made in a place where inspectors get a two-month heads-up… i’m not just mad. i’m heartbroken.
why do we let profit dictate safety? why don’t we treat medicine like we treat airplane parts? because if a plane part is made poorly, someone dies. same with pills. but we’re just… shrugging?
also, i’m so tired of people saying ‘india makes it cheaper.’ yeah, but at what cost? my grandma almost died from a contaminated batch. it wasn’t ‘a few bad apples.’ it was a systemic failure.
thank you for writing this. i’m sharing it with everyone i know.
as a guy who’s lived in both the US and india, i’ve seen how hard these factories work. people are proud of their jobs. they want to make good medicine. but the system? it’s broken. not because they’re lazy or dishonest-but because they’re trapped.
the old rules rewarded short-term fixes. now? they have to build real systems. that’s hard. expensive. scary.
but if we treat them like partners, not suspects, we can make this work. train them. support them. don’t just threaten them.
also-can we please stop calling india and china the ‘bad guys’? they’re not villains. they’re players in a global game we designed poorly. let’s fix the game, not blame the players.
the statistical disparity in violation rates between domestic and foreign facilities is not surprising given the inspection frequency differential. prior to 2025, the probability of detection for foreign facilities was significantly lower due to scheduled inspections, which permitted temporal remediation. the introduction of unannounced inspections reduces this bias and improves the validity of compliance assessments.
the proposed qualified person model aligns with eu regulatory philosophy and may enhance accountability. however, implementation challenges include legal jurisdiction and liability frameworks.
hey, i just checked my bottle of metformin-made in india. i’m not mad, i’m just… curious. do you think they’re still backdating logs? or did they finally get the memo?
also, can someone explain why the FDA lets companies ship drugs even after they’ve been warned? like, what’s the point of a warning if you just keep selling?
the FDA’s shift toward unannounced inspections is a necessary and proportionate response to documented systemic deficiencies in foreign manufacturing oversight. the prior inspection regime created a moral hazard, incentivizing performative compliance rather than sustained adherence to cGMP standards.
the proposed qualified person model, while administratively complex, introduces a critical locus of legal accountability that is currently absent. this is a step toward harmonizing safety expectations across borders.
the increase in inspection capacity, while commendable, must be matched with transparent public reporting and independent audit mechanisms to prevent regulatory capture.
my mom takes 7 pills a day. none of them say where they’re made. i just found out two of them came from a plant that got a warning letter last year. i’m gonna call her pharmacist tomorrow. thanks for making me care about this.