Medication Interaction Checker
Check Your Medication Safety
Identify dangerous combinations between your respiratory medications and other drugs. This tool helps you recognize interactions that could affect your breathing.
Interaction Results
After selecting your medications, results will appear here.
When you're managing asthma or COPD, your inhaler isn't the only thing that affects your breathing. Many of the pills, creams, and over-the-counter remedies you take every day can quietly sabotage your lung function - sometimes with life-threatening results. This isn't theoretical. Real people are ending up in emergency rooms because they didn't know that their headache medicine, sleep aid, or heart pill could trigger a severe asthma attack or cause their oxygen levels to crash. If you or someone you care about is on respiratory medication, you need to understand what’s really going on - not just what the label says, but what your body is experiencing behind the scenes.
What Medications Are You Really Taking?
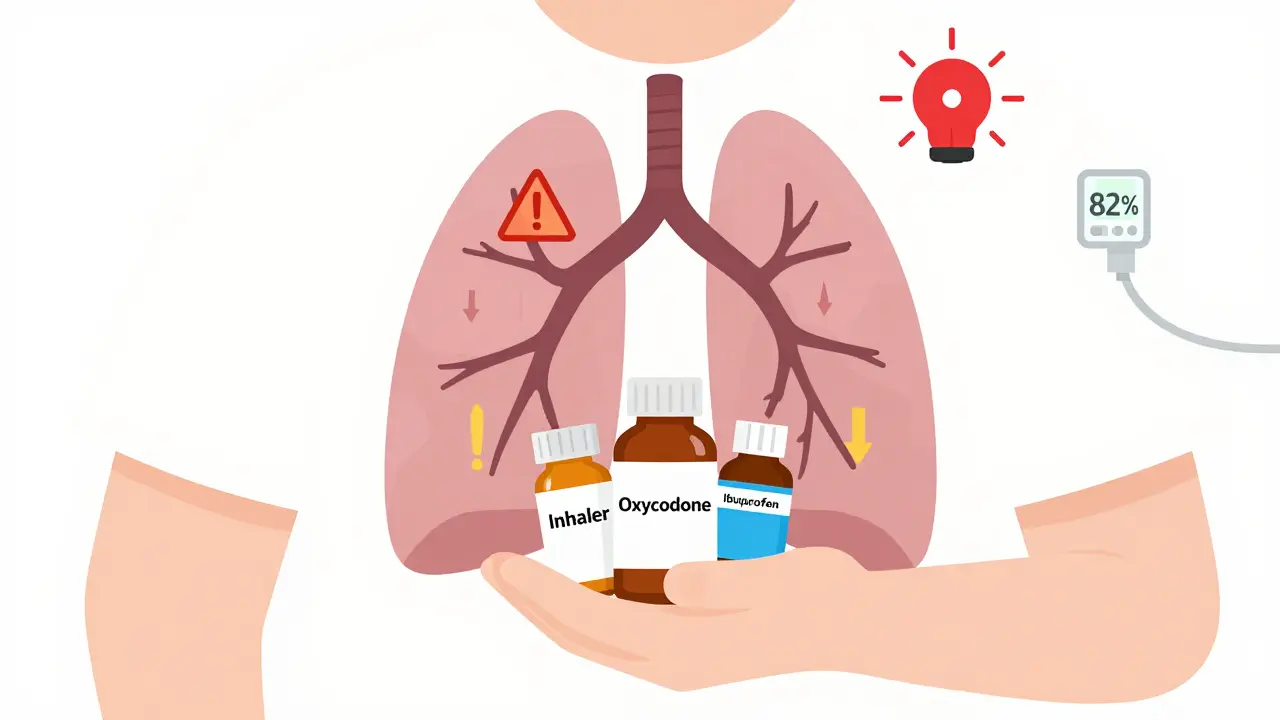
Most asthma and COPD patients are on multiple drugs at once. That’s not unusual. But the problem isn’t the number of medications - it’s the hidden combinations. You might be taking a long-acting beta-agonist (LABA) like formoterol to keep your airways open, a long-acting muscarinic antagonist (LAMA) like tiotropium to relax smooth muscle, and an inhaled corticosteroid to reduce inflammation. All three are standard. But then you add a painkiller, an antihistamine, or a heart medication - and suddenly, things go sideways.The most dangerous combinations aren’t always obvious. Take opioids. If you have COPD and are prescribed oxycodone for back pain, that’s not inherently unsafe - unless you’re also taking diphenhydramine (Benadryl) for allergies or sleep. The FDA’s own adverse event database shows that 17% of opioid-related hospitalizations in COPD patients involved this exact combo. Both drugs slow breathing. Together, they can drop your oxygen saturation to dangerously low levels - like 82% - without warning. One patient in a COPD support group described waking up gasping after taking both. She didn’t realize either was risky. Neither did her doctor.
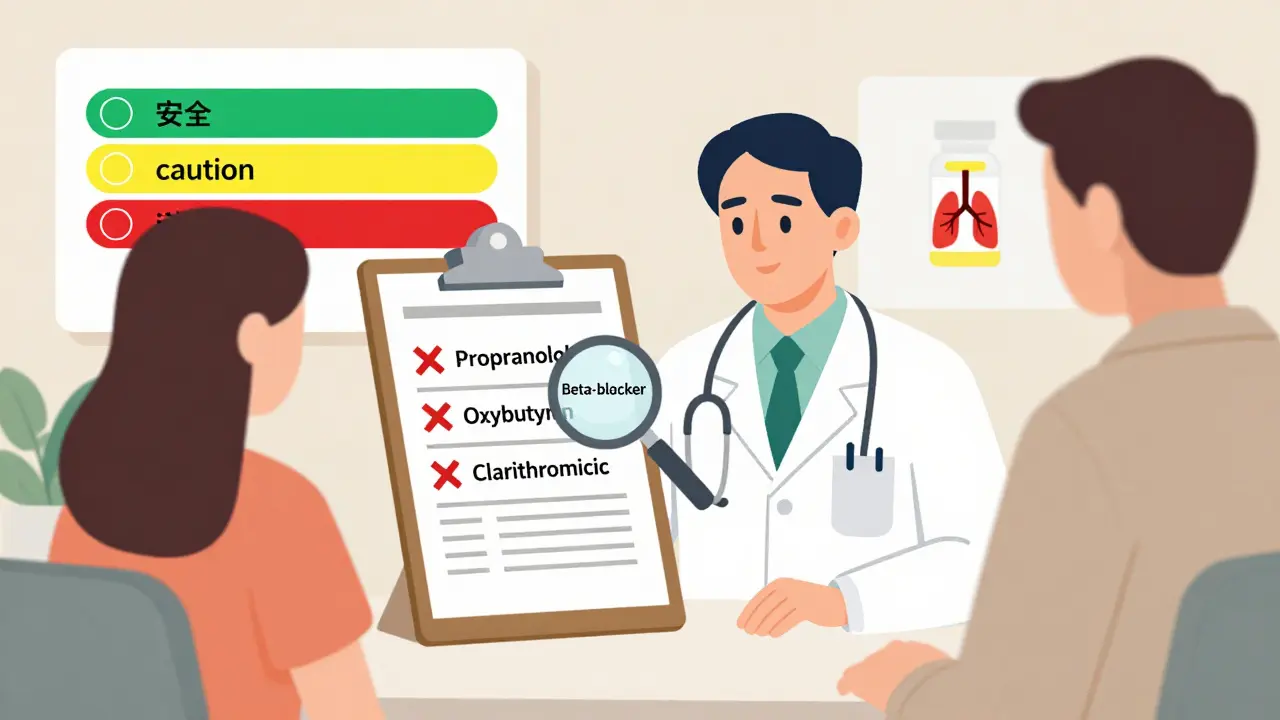
Then there’s the beta-blocker trap. If you have asthma and are prescribed propranolol for high blood pressure, you’re at serious risk. Propranolol blocks beta-2 receptors in your lungs - the very receptors your inhaler relies on to open your airways. Studies show this can reduce your FEV1 (a key lung function measure) by 15-25%. That’s not a small dip. That’s enough to trigger a full-blown attack. Even worse, many patients don’t know they’re on a nonselective beta-blocker. The label says “metoprolol” - which is safer - but if your prescription was switched without explanation, you might be on the dangerous kind. Always ask: “Is this a selective or nonselective beta-blocker?”
NSAIDs and Aspirin: The Silent Triggers
If you have asthma - especially with nasal polyps or chronic sinusitis - you’re part of a group that’s 10% more likely to react badly to common pain relievers. Ibuprofen, naproxen, aspirin - even a single tablet can cause your airways to tighten within an hour. It’s not an allergy. It’s a pharmacological reaction. The body responds by producing excess leukotrienes, which cause inflammation and bronchoconstriction. One Reddit user, “BreathingHard2020,” posted about a near-fatal attack after taking Advil for a migraine. He’d never connected the dots until his pulmonologist asked about OTC meds. Now he keeps a list. So should you.And here’s the kicker: doctors rarely ask. A 2023 survey by Asthma + Lung UK found that 68% of patients who had medication-related breathing issues didn’t mention their non-respiratory drugs to their provider. Why? Because they assume it’s “just a painkiller.” It’s not. It’s a potential trigger.
The Anticholinergic Trap
LAMA inhalers like tiotropium and glycopyrrolate are lifesavers for COPD. But they’re also anticholinergics - meaning they block a nerve signal that tightens airways. The same mechanism helps with overactive bladder. So if you’re taking oxybutynin for urinary urgency, you’re doubling down on anticholinergic effects. The result? Dry mouth, constipation, urinary retention - and worse, confusion and dizziness in older adults. A 2023 European Respiratory Society paper found a 28% spike in acute urinary retention among male COPD patients taking both a LAMA and a bladder medication. That’s not rare. That’s predictable.And it’s not just bladder meds. Antihistamines like diphenhydramine (Benadryl), tricyclic antidepressants like amitriptyline, and even Parkinson’s drugs like benztropine all carry the same warning. They’re not just “mild side effects.” They’re cumulative. One patient on Reddit described feeling “drunk” after adding a nighttime allergy pill to his COPD regimen. His oxygen monitor didn’t show a drop - but his confusion did. That’s the hidden cost.
Antibiotics and Antifungals: The Unseen Interferers
Clarifying a common myth: antibiotics don’t directly cause asthma attacks. But some - like clarithromycin - interfere with how your liver processes your inhalers. Clarithromycin blocks the CYP3A4 enzyme, which breaks down many LABAs and corticosteroids. The result? Your medication builds up in your system. You get more side effects: tremors, rapid heartbeat, even heart rhythm problems. The same goes for antifungals like ketoconazole. A 2022 study in the Journal of the American Pharmacists Association showed that pharmacists who reviewed prescriptions for COPD patients caught these interactions in 43% of cases. That’s nearly half of all patients at risk - and most didn’t know.And here’s what’s rarely said: some antibiotics can worsen COPD by triggering inflammation. Azithromycin, for example, is sometimes used long-term to prevent flare-ups - but it’s not harmless. It can cause QT prolongation, a heart rhythm issue that’s dangerous when combined with other drugs. Always ask: “Is this antibiotic safe with my other meds?”
What You Can Do Right Now
Knowledge is power - but only if you act on it. Here’s what works:- Keep a real-time medication list. Not a mental list. Not a scrap of paper. Write down every pill, inhaler, patch, cream, supplement, and OTC drug - including doses and why you take them. Update it after every doctor visit.
- Do the brown bag test. Once a year, bring every medication you take - in the original bottles - to your doctor or pharmacist. Don’t leave anything out. Not the melatonin. Not the ibuprofen. Not the cough syrup.
- Ask three questions at every appointment:
- “Could this new medication interact with my asthma or COPD drugs?”
- “Is there a safer alternative if I’m already on a beta-blocker or anticholinergic?”
- “Should I be tested for NSAID sensitivity?”
- Use the COPD Medication Safety App. Launched in 2023 by the COPD Foundation, it checks 95% of commonly used drugs for interactions with respiratory meds. It’s free. It works offline. And it’s updated monthly.
The American Lung Association’s Medication Safety Action Plan includes a color-coded chart: green for safe, yellow for caution, red for avoid. Print it. Tape it to your fridge. Share it with your family. You’re not being paranoid - you’re being smart.
Why This Matters More Than Ever
By 2026, over 470 million people worldwide are living with asthma or COPD. And as populations age, more of them are on five, six, even ten medications. Polypharmacy isn’t a buzzword - it’s a growing crisis. A 2022 study found that 37% of moderate-to-severe COPD patients were taking at least one drug that could worsen their condition. That’s not a glitch. That’s a system failure.The good news? Change is happening. The FDA’s Sentinel Initiative now actively tracks respiratory drug interactions. The European Medicines Agency is updating label warnings for all new respiratory meds. Electronic health records are being programmed to flag dangerous combos before they’re prescribed. But none of that helps you - unless you know what to look for.
Your lungs don’t care about medical guidelines. They care about what’s in your bloodstream. And if you’re not checking every pill you take, you’re gambling with your breathing.
Can I still take ibuprofen if I have asthma?
If you have asthma - especially with nasal polyps or chronic sinusitis - ibuprofen and other NSAIDs can trigger a severe bronchoconstriction reaction. About 10% of adult asthmatics are sensitive to these drugs. Symptoms can appear within 30 to 120 minutes and include wheezing, shortness of breath, or a full asthma attack. If you’ve ever had breathing trouble after taking a painkiller, avoid NSAIDs. Use acetaminophen (paracetamol) instead. Always test with your doctor before assuming it’s safe.
Are all beta-blockers dangerous for asthma patients?
No. Nonselective beta-blockers like propranolol and nadolol are dangerous because they block beta-2 receptors in the lungs, which can cause severe bronchospasm. But selective beta-blockers like metoprolol, atenolol, or bisoprolol mainly affect the heart and are generally safe for mild to moderate asthma. Studies show only 2-5% of asthma patients on selective beta-blockers experience breathing issues. Still, always start at a low dose and monitor closely. Never take a beta-blocker without discussing it with your pulmonologist.
Can I take Benadryl if I have COPD?
Diphenhydramine (Benadryl) is an antihistamine with strong anticholinergic effects. For COPD patients, it can worsen dry mouth, constipation, urinary retention, and confusion. More critically, it can slow breathing - especially if combined with opioids or LAMA inhalers. The FDA has documented cases of oxygen saturation dropping below 85% in COPD patients who took Benadryl with oxycodone. Safer alternatives include loratadine (Claritin) or cetirizine (Zyrtec), which have minimal anticholinergic activity. Avoid Benadryl unless absolutely necessary and under medical supervision.
What should I do if I’m on multiple inhalers and a new prescription?
Always bring your complete medication list - including all inhalers - to your pharmacist or doctor before starting any new drug. Many drug interactions occur between respiratory and non-respiratory medications. For example, combining a LAMA like tiotropium with an anticholinergic bladder drug like oxybutynin increases your risk of urinary retention by 28%. Use the COPD Medication Safety App to check for interactions before taking a new pill. If you’re unsure, delay the new medication until you’ve consulted a specialist.
How common are medication-related asthma or COPD emergencies?
According to the International Journal of Chronic Obstructive Pulmonary Disease, inappropriate drug combinations contribute to 15-20% of COPD-related hospitalizations. A 2023 Asthma + Lung UK survey found that 31% of respondents had experienced breathing problems linked to non-respiratory medications. In the U.S., the FDA’s Adverse Event Reporting System shows that over 2,000 COPD-related emergency cases between 2020 and 2022 involved drug interactions - mostly from opioids, antihistamines, and antibiotics. These aren’t rare events. They’re preventable.