Every day, pharmacists dispense millions of generic drugs. They’re the last checkpoint before a patient takes their medication. But when something goes wrong-a patient has a strange reaction, a pill doesn’t work like it used to, or a generic version causes unexpected side effects-pharmacist responsibility for reporting generic drug problems isn’t just good practice. It’s a critical part of keeping the drug supply safe.
Why Pharmacists Are the Frontline for Generic Drug Safety
Pharmacists see what doctors don’t. They watch patients pick up refills. They notice when a patient says, "This new pill makes me dizzy," or "I used to take this generic and it worked fine, but now I’m crashing after an hour." These aren’t just complaints. They’re signals. And they’re often the first signs of a deeper problem. The FDA doesn’t require pharmacists to report adverse events, but it strongly encourages it. The agency’s MedWatch program is designed for exactly this: real-world observations from people who interact with drugs daily. Pharmacists are uniquely positioned to spot issues like therapeutic inequivalence-when a generic drug doesn’t perform the same way as the brand version, even though it’s legally approved. This isn’t about quality control alone. It’s about whether the drug actually works the same in real people. In 2022, the FDA received over 28,000 reports mentioning generic drug problems. That’s up from just over 12,000 in 2015. But here’s the problem: less than 3% of those reports came from pharmacists. Meanwhile, pharmacists dispense about 75% of all prescriptions in the U.S.-and nearly 90% of those are generics. That means for every 100 generic drugs a pharmacist hands out, they’re seeing problems that could be reported, but most of the time, they’re not.What Counts as a Reportable Problem?
Not every side effect needs to be reported. The FDA defines serious adverse events as those that are:- Life-threatening
- Result in hospitalization
- Cause permanent disability
- Lead to birth defects
- Require medical intervention to prevent serious harm
- Identifiable patient (age, gender, initials are enough)
- The drug name and National Drug Code (NDC)
- The manufacturer and lot number
- A clear description of the event
- When it happened and what the patient was doing
The Hidden Problem: Who’s to Blame?
Here’s where it gets messy. Generic manufacturers are legally required to use the same labeling as the brand-name drug. They can’t update warnings on their own-even if they know something’s wrong. That’s because of a 2011 Supreme Court decision, PLIVA v. Mensing, which ruled that generic manufacturers can’t be sued for failing to warn patients. The court said federal law preempts state tort claims. The result? Generic manufacturers have little incentive to report problems. They don’t control the label. They don’t face liability. So they wait for someone else to report it. And who does that? Usually, the brand-name manufacturer-because they’re the ones who originally got the FDA approval. But if a patient took a generic, how does the brand company even know? That’s where pharmacists come in. They’re the only ones who know exactly which product was dispensed. When a patient says, "I got the generic from CVS," and then has a reaction, the pharmacist is the only one who can trace it to the right manufacturer. Without that information, the FDA can’t tell if it’s a problem with one batch, one company, or a systemic flaw.
Why Don’t Pharmacists Report More?
It’s not that they don’t care. A 2023 survey of community pharmacists found that 89% believe reporting adverse events is part of their professional duty. But only 44% actually do it regularly. The top reasons?- 68% say they don’t have time
- 52% aren’t sure if the event meets reporting criteria
- 42% can’t tell if the problem came from the brand or the generic
Real-World Impact: What Happens When Reports Are Made?
In 2022, the FDA’s Office of Generic Drugs reviewed 147 drug products based on pharmacist-submitted reports. Twelve of those led to direct communications to healthcare providers about potential safety issues. That’s not a small number. That’s a lifesaving intervention. One example: pharmacists in several states noticed patients on a generic version of levothyroxine were experiencing fatigue, weight gain, and heart palpitations-symptoms that didn’t happen with the brand version. The reports piled up. The FDA investigated. They found that the generic had inconsistent dissolution rates. The manufacturer had to change its formula. Thousands of patients avoided worsening thyroid conditions because pharmacists spoke up. Another case involved a generic antiepileptic drug. Multiple pharmacists reported patients having breakthrough seizures after switching. The FDA pulled the product from the market. No one died. But many could have. These aren’t hypotheticals. They’re real outcomes from real reports.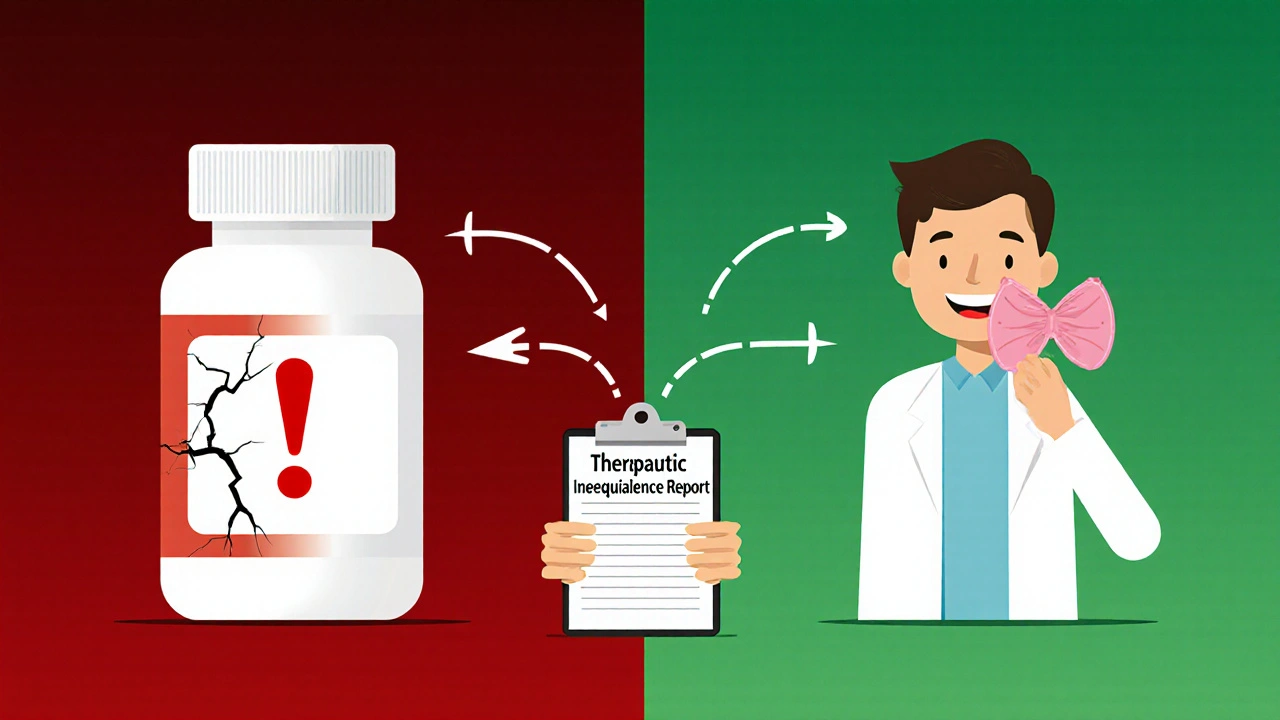
What You Can Do: A Simple Reporting Checklist
You don’t need to be an expert to report. Here’s a quick guide:- When a patient reports a change after switching to a generic, ask: "When did you start the new version?" and "What’s different now?"
- Check the prescription label. Write down the manufacturer name and NDC code.
- Use the FDA’s MedWatch online portal (version 3.2 or later). There’s now a "generic drug concern" dropdown-choose "therapeutic inequivalence," "manufacturing issue," or "labeling problem."
- Include: patient age, event description, timing, and whether it happened after a switch.
- Submit even if you’re unsure. The FDA says: "Report if you suspect it might be related."
State Rules Are Changing-Are You Ready?
While federal law doesn’t require reporting, 28 states have included reporting expectations in their pharmacy board regulations. Four states-California, Illinois, Massachusetts, and New York-have made it mandatory to report serious adverse events. If you practice in one of those states, you’re not just being helpful. You’re complying with the law. Even if you’re not in one of those states, professional guidelines from the American Society of Health-System Pharmacists (ASHP) and the Institute for Safe Medication Practices (ISMP) treat reporting as a core responsibility. Your license isn’t just about dispensing pills. It’s about protecting patients from hidden risks.What’s Next for Generic Drug Safety?
The FDA is pushing for more pharmacist involvement. Their 2022 Modernization Act specifically encouraged reports of therapeutic inequivalence. The Office of Generic Drugs now has a dedicated working group to analyze pharmacist-submitted data. They’re listening. But they can’t fix what they don’t know. And they won’t know unless pharmacists start reporting. This isn’t about blame. It’s about accountability. Pharmacists are the bridge between the drug and the patient. When something goes wrong, they’re the ones who see it first. That’s not a burden. It’s a responsibility-and one that can save lives.Are pharmacists legally required to report generic drug problems?
No, federal law does not require pharmacists to report adverse events or generic drug issues. However, the FDA strongly encourages reporting through the MedWatch program, and some states like California, Illinois, Massachusetts, and New York have made it mandatory to report serious adverse events. Professional organizations like ASHP and ISMP also treat reporting as a core ethical and professional duty.
What types of generic drug problems should I report?
Report serious adverse events-like hospitalizations, life-threatening reactions, or permanent disability. Also report therapeutic inequivalence: when a generic drug doesn’t work the same as the brand version, even if it’s approved as bioequivalent. Examples include uncontrolled seizures, unstable thyroid levels, or sudden drops in blood pressure after switching generics. Even if you’re unsure, report it. The FDA says: "If you suspect it might be related, submit the report."
How do I know which manufacturer made the generic drug?
Check the prescription label or the bottle. The manufacturer name and National Drug Code (NDC) are printed on the packaging. If you’re unsure, contact the wholesaler or use the FDA’s NDC Directory online. Accurate manufacturer info is critical-without it, the FDA can’t trace the problem to the right company.
Can I report if I don’t have the lot number?
Yes, you can still report without the lot number. The FDA accepts reports without it, but including it greatly improves the chances of identifying a batch-specific issue. If you don’t have it, write "unknown" or "not available." Better to report with partial info than not at all.
How long do I have to report a serious adverse event?
The FDA requires serious adverse events to be reported within 15 calendar days of first receiving the information. While this isn’t legally binding for pharmacists, meeting this timeline helps ensure timely safety reviews. Non-serious but unexpected events should be reported as soon as possible to help detect new safety signals.
Why do so few pharmacists report compared to doctors?
Doctors prescribe more often and may be more familiar with reporting systems. Pharmacists face time constraints, uncertainty about what to report, and difficulty identifying which manufacturer’s product caused the issue. Also, there’s no financial incentive or formal tracking system in most pharmacies. Despite dispensing 90% of generics, pharmacists contribute less than 3% of reports to the FDA.
Is there training available for pharmacists on how to report?
Yes. The FDA offers free online training through the MedWatch Training Portal. Module 4: "Reporting for Healthcare Professionals" (updated January 2023) includes specific guidance on reporting generic drug issues, including therapeutic inequivalence. The American Pharmacists Association and ASHP also provide resources and templates to help streamline reporting.

Man, I’ve seen this so many times. Patient comes in, says their generic levothyroxine is making them feel like a zombie. We switch ‘em back to brand, they’re fine. But reporting? Nah, no time. We’re running on fumes between refills and insurance calls. Feels like we’re the only ones who notice, but no one listens.
While the intent behind encouraging pharmacist reporting is commendable, the absence of a standardized, incentivized reporting mechanism undermines its efficacy. The current system places undue administrative burden on professionals already operating under significant time constraints.
It is my professional opinion that pharmacists, as custodians of medication safety, bear an ethical obligation to report adverse events, irrespective of regulatory mandates. The absence of legal compulsion does not negate the moral imperative to act in the interest of public health.
Look, the whole generic drug system is a regulatory circus. Brand companies get the original approval, then generic makers copy the formula but can’t update the label even if they find out the damn thing’s causing seizures. Supreme Court ruling in PLIVA v. Mensing? Total legal loophole. Pharmacists are stuck in the middle-watching patients suffer, knowing which batch caused it, but the manufacturer doesn’t care because they can’t be sued. Meanwhile, the FDA’s MedWatch form is like filling out a tax return in 1987-no auto-fill, no mobile app, just a clunky webpage that crashes if you blink wrong. And don’t even get me started on how the NDC codes change every time a wholesaler repackages. We’re not just reporting side effects-we’re doing detective work with half the data.
My grandma switched generics last month and started passing out. We caught it before she fell down the stairs. I printed out the MedWatch form and filled it out in 8 minutes. Took her to the doc, we got the NDC off the bottle. Easy. Why don’t more people just do this? It’s not hard.
The 3% reporting rate from pharmacists is statistically insignificant given the volume of prescriptions dispensed. This suggests either systemic apathy or a fundamental flaw in the incentive structure. The FDA’s reliance on anecdotal reporting is not a robust pharmacovigilance strategy-it’s a stopgap.
Let’s be real-pharmacists are the unsung heroes of drug safety. We’re the ones who catch the weird stuff before it becomes a headline. That levothyroxine case? That’s why I started documenting every odd reaction on a sticky note in my pocket. Now I’ve got a whole notebook. I don’t wait for the FDA to ask-I just send it. And you know what? Someone at the agency actually replied to one of mine last year. They said, ‘We’re looking into this.’ That’s all it takes. One report. One person who cares. You don’t need a degree in pharmacology to do this. You just need to care enough to type it out.
I’ve been a pharmacist for 18 years. I’ve seen too many patients confused, scared, and ignored. Reporting feels like shouting into a void. But I still do it. Not because I expect change. Because I owe it to the people who trust us with their health. Even if it’s just one report. Even if no one ever sees it. It matters.
Who even reads these reports? The FDA is just another bureaucracy that collects dust. They’ve got a whole team of interns sifting through 28k reports a year. Half of them are probably just people blaming generics for their hangovers. And don’t get me started on the NDC codes-half the time the bottle says one thing, the system says another. This whole system is a joke. Why don’t we just make every drug brand-only? At least then we’d know who to yell at.
I’ve been quietly reporting every time I see a pattern-three patients on the same generic metformin with sudden nausea, or two with the same generic warfarin with INR spikes. I don’t say anything in front of patients. I just write it down. I’ve submitted 14 reports in the last year. No one’s ever called me back. But I keep doing it. I guess I’m hoping someone’s listening. Or maybe I’m just trying to feel like I’m not just a pill dispenser.
THIS IS A BIG PHARMA COVER-UP. THEY KNOW THE GENERICS ARE SHIT. THEY’RE USING CHEAP FILLERS LIKE TALC AND BORAX TO SAVE MONEY. THE FDA IS IN THEIR POCKET. THEY DON’T WANT YOU TO KNOW THAT YOUR THYROID MED IS MADE IN A FACTORY THAT USED TO MAKE TOILET CLEANER. I SAW A LOT NUMBER ON A BOTTLE ONCE-IT MATCHED A RECALL FROM 2019. I REPORTED IT. THEY IGNORED IT. NOW I’M DOING A YOUTUBE SERIES. WATCH OUT.
The discrepancy between pharmacist reporting rates and prescription volume is not merely a procedural issue-it is indicative of a structural failure in the pharmacovigilance ecosystem. The absence of a mandated, digitized, and integrated reporting interface within pharmacy management systems constitutes a critical oversight.
wait i just realized i never checked the lot number on my meds… oops. i think i have a bottle at home from last month… lemme go look. i’ll report if i find something weird. i swear i’m not lazy, i just… forget. sorry.