Living with IBS-Mixed means your body doesn’t settle into a pattern. One day you’re stuck on the toilet with hard, painful stools. The next, you’re racing to the bathroom with watery diarrhea. It’s not just inconvenient-it’s exhausting. And if you’ve been told it’s "just stress" or "you’re overreacting," you know that’s not true. IBS-Mixed, or IBS-M, is a real, diagnosable condition affecting about 20-25% of all IBS patients. Unlike IBS-C or IBS-D, where constipation or diarrhea dominates, IBS-M flips between both. That makes treatment tricky. What helps one day can make things worse the next. But there’s a way through it.
What Exactly Is IBS-Mixed?
IBS-Mixed isn’t just "IBS that acts up." It’s defined by strict medical criteria: abdominal pain at least once a week for three months, linked to changes in bowel habits. You must have both hard or lumpy stools (Bristol Scale 1-2) and loose or watery stools (Bristol Scale 6-7) in at least 25% of your bowel movements. This isn’t random. It’s a pattern. And it’s recognized by the Rome IV guidelines, the gold standard for diagnosing IBS since 2016.
What sets IBS-M apart from Crohn’s or ulcerative colitis? No inflammation. No ulcers. No bleeding. Your colon looks normal on a scope. But your gut is hypersensitive. Your nerves are on edge. Your muscles contract too fast or too slow. And your gut bacteria are out of balance. This isn’t in your head-it’s in your gut-brain axis.
Why Is IBS-M So Hard to Treat?
Imagine trying to fix a car that sometimes won’t start and other times revs too high. That’s IBS-M. Laxatives help constipation but trigger diarrhea. Anti-diarrheals like loperamide calm loose stools but can make you painfully backed up. A 2018 study showed that drugs like linaclotide (used for IBS-C) only helped 22% of IBS-M patients-far less than in IBS-C. Same with eluxadoline for IBS-D: it worked for 38% of those patients, but only 19% of IBS-M.
That’s why most people with IBS-M end up juggling two medications: one for constipation, one for diarrhea. It’s not ideal, but it’s often necessary. A 2022 survey found that 65% of IBS-M patients had to adjust their meds monthly based on what their gut was doing that week. And it’s not just drugs. Food plays a huge role. Dairy triggers symptoms in 28% of people. Caffeine? 24%. High-fat meals? 22%. Stress? 68% say it makes everything worse.
The Low FODMAP Diet: Your Best Shot at Stability
If you’ve tried cutting out gluten or dairy and nothing changed, you’re not alone. But the low FODMAP diet has real science behind it. It doesn’t work for everyone, but it helps about 50-60% of IBS-M patients-slightly less than for IBS-D, but still the most effective dietary tool we have.
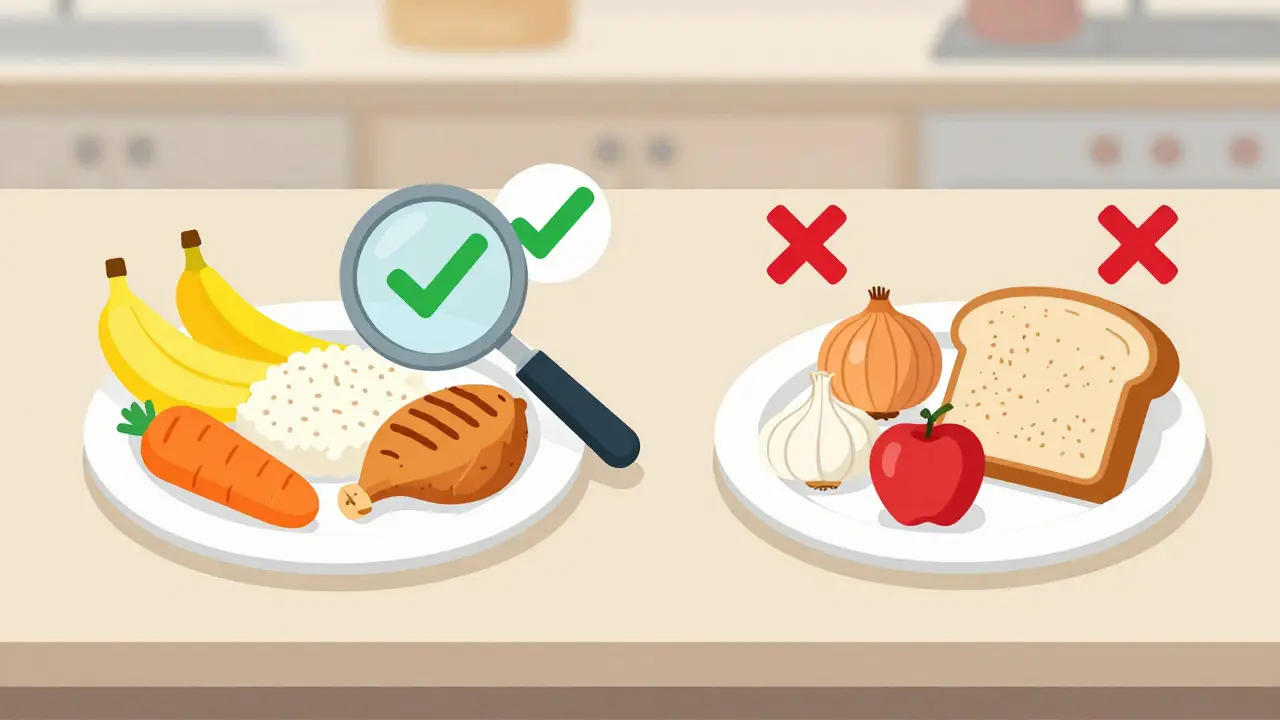
FODMAPs are short-chain carbs that ferment in your gut and pull water in, causing bloating, gas, and changes in bowel speed. High-FODMAP foods include onions, garlic, apples, wheat, milk, and beans. The diet has three phases: elimination (2-6 weeks), reintroduction (8-12 weeks), and personalization.
Here’s the key: you don’t stay on the strict version forever. You test foods one by one to find your triggers. A 2021 trial with 215 patients showed those who followed the diet with a dietitian had a 60% drop in symptom severity. Reddit users report similar results-many say they went from 25 symptom days a month to under 10 after 3 months. But doing it alone? That’s where most fail. A registered dietitian who specializes in IBS is worth every dollar.
Medications That Actually Work for IBS-M
No drug is FDA-approved specifically for IBS-M. That means doctors have to be creative. Here’s what works based on evidence:
- Antispasmodics (like dicyclomine 10-20mg as needed): Reduce cramping and spasms. Help 40-50% of users, regardless of whether they’re constipated or diarrhea-predominant.
- Low-dose antidepressants (TCAs like amitriptyline 10-50mg at night): These aren’t for depression. They calm gut nerves and reduce pain signals. Studies show 55-60% of IBS-M patients improve with TCAs-better than any other subtype.
- Psyllium husk (5g daily): A soluble fiber that smooths out bowel movements. It absorbs water in diarrhea and softens stool in constipation. One study found 52% of IBS-M users had consistent relief with psyllium + dicyclomine.
- Enteric-coated peppermint oil (IBgard): Reduces bloating and pain. 68% of users report less discomfort. Avoid if you have heartburn-it can trigger reflux.
- For constipation: Polyethylene glycol (Miralax, 17g daily) is gentle and doesn’t cause rebound diarrhea.
- For diarrhea: Loperamide (Imodium, 2-4mg as needed) works fast. But don’t use daily-it can worsen constipation over time.
Never take both laxatives and anti-diarrheals at the same time. Keep them separate. Use one only when needed. Track what works. That’s how you learn your rhythm.
Stress Isn’t the Cause-But It’s the Fuel
You’ve heard it before: "It’s all in your head." But here’s the truth: stress doesn’t cause IBS-M. But it turns up the volume. Your gut has its own nervous system-200 million neurons. When you’re anxious, your brain sends signals that make your gut hypersensitive. Pain feels worse. Contractions get erratic.
Cognitive Behavioral Therapy (CBT) isn’t a luxury-it’s a medical treatment. A 2021 guideline from the American Gastroenterological Association gave CBT a strong recommendation for IBS-M. In 12 trials, CBT reduced symptom severity by 40-50%. That’s better than most drugs. Apps like Cara Care and The IBS Clinic offer structured CBT programs you can do at home. Even 8-10 sessions can change your relationship with your gut.
Other stress tools: daily breathing exercises, yoga, walking in nature. Not because they’re trendy-but because they lower your body’s fight-or-flight response. And that directly calms your gut.
What to Track (And How to Do It Right)
Guessing what triggers your symptoms? You’re flying blind. Tracking is non-negotiable. Use a simple system:
- Bristol Stool Scale (1-7): Write down the number each time you go.
- Pain level: 0-10 scale. Note if it’s cramping, burning, or bloating.
- Food: What you ate 24 hours before symptoms started.
- Stress: Was it a bad day at work? A fight? Lack of sleep?
- Medication: What you took and when.
Use an app like Cara Care or IBS Symptom Tracker. A 2022 study found people using apps improved 35% more than those using paper diaries. You’re not just logging data-you’re finding patterns. Maybe your pain spikes after coffee on Mondays. Or you’re fine until you eat pizza on Friday nights. That’s power.
What Doesn’t Work (And Why)
There’s a lot of noise out there. Here’s what to avoid:
- Gluten-free without a diagnosis: Only helps if you have celiac disease (which you can rule out with a blood test).
- Probiotics without knowing the strain: Most are useless. Only specific strains like Bifidobacterium infantis 35624 (Align) have evidence for IBS-M.
- Overdoing fiber: Insoluble fiber (wheat bran, nuts) can make diarrhea worse. Stick to soluble fiber like psyllium.
- Detox teas and colon cleanses: They irritate your gut and disrupt your microbiome. No benefit. Only risk.
- Waiting for a "magic pill": There isn’t one. IBS-M management is a lifestyle, not a quick fix.
What’s Coming Next
The future is personal. In 2023, the FDA approved ibodutant, a new drug that showed 45% symptom improvement in IBS-M patients-nearly double placebo. It’s not on the market yet, but it’s coming. Viome’s AI gut test analyzes your microbiome and gives you a custom diet plan. In a pilot study, 58% of users saw big improvements. And the Rome Foundation is updating criteria in 2024 to require alternating symptoms in 30% of bowel movements-making diagnosis even more precise.
But the biggest breakthrough won’t be a pill. It’ll be access. Right now, IBS-M diagnosis is delayed by 6-7 years. Racial minorities and rural patients are diagnosed 30% less often. If you’re struggling, don’t wait. Bring your symptom log to your doctor. Ask for a referral to a GI specialist or dietitian. You deserve care that matches your reality.
You’re Not Alone
IBS-M is messy. It’s unpredictable. It steals your confidence. But you’re not broken. You’re not lazy. You’re not imagining it. You’re managing a complex system that’s out of sync-and you’re learning how to tune it. It takes time. Most people see real improvement after 3-6 months of consistent tracking, diet tweaks, and stress management. Don’t give up. Small changes add up. One less trigger. One better night’s sleep. One day without panic about the nearest bathroom. That’s progress.
Can IBS-Mixed turn into Crohn’s disease or ulcerative colitis?
No. IBS-M is a functional disorder, meaning there’s no structural damage or inflammation in your gut. Crohn’s and ulcerative colitis are inflammatory diseases with visible tissue damage. IBS-M doesn’t progress into them. But if you notice blood in your stool, unexplained weight loss, or fever, see a doctor immediately-those aren’t IBS symptoms.
Why do I feel fine on weekends but terrible on workdays?
Stress is the biggest clue. Workdays often mean rushed meals, caffeine, skipped breaks, and emotional pressure-all IBS triggers. Weekends might bring slower routines, better sleep, and less anxiety. Tracking your stress levels alongside symptoms will reveal this pattern. CBT and mindfulness can help rewire your response.
Is it safe to take loperamide every day?
No. Loperamide is meant for short-term use during diarrhea flares. Daily use can lead to constipation, bloating, and even dangerous bowel slowdown. Use it only when you need it-2-4mg max per day, no more than 3-4 days in a row. Let your body regulate itself between episodes.
What’s the best fiber supplement for IBS-Mixed?
Psyllium husk (Metamucil, Konsyl) is the gold standard. It’s soluble, gentle, and balances both constipation and diarrhea. Start with 5g daily, mixed in water. Increase slowly. Avoid wheat bran or inulin-they’re insoluble and often make symptoms worse.
Can I ever eat normally again?
Yes. The low FODMAP diet isn’t forever. After the elimination and reintroduction phases, most people find a personal list of tolerable foods. You might still avoid onions or apples, but you can enjoy many things you thought were off-limits. The goal isn’t restriction-it’s freedom through knowledge.
Why do some doctors dismiss IBS-M?
Because it’s invisible. No blood test, no scan, no biopsy confirms it. Some doctors don’t have the time or training to manage complex functional disorders. But you’re not alone-65% of IBS-M patients report feeling misunderstood. Bring your symptom log, cite the Rome IV criteria, and ask for a referral to a gastroenterologist or dietitian who specializes in IBS. You deserve better.

Been managing IBS-M for 8 years. The psyllium husk tip changed everything. Started with 5g, slowly increased. No more panic attacks before leaving the house. It’s not magic, but it’s the closest thing I’ve found to balance.
Also, CBT via Cara Care-10 sessions, and my stress-response gut reactions dropped by half. Not because I’m "overreacting," but because my nervous system finally stopped screaming at me.
People who say "it’s just anxiety" don’t get it. It’s real. It’s physical. And you’re not broken for needing help.
Also, peppermint oil capsules? Lifesaver. Just don’t take them if you get heartburn. Learned that the hard way.
Let’s be crystal clear: IBS-M isn’t a "diet problem." It’s a neuro-gastrointestinal dysregulation with microbiome modulation as a secondary lever. The Rome IV criteria are non-negotiable for diagnosis, and anyone who conflates it with SIBO or celiac is operating on outdated, reductive models.
Psyllium is indeed superior to insoluble fiber-not because it’s trendy, but because its hydrophilic colloidal properties modulate transit time bidirectionally. The 2021 trial data is robust. But here’s the kicker: the real win is personalized reintroduction. You don’t eliminate FODMAPs forever-you engineer your own symphony of tolerance.
And yes, low-dose TCAs work better than SSRIs for IBS-M. Not because they’re antidepressants, but because they dampen visceral hypersensitivity via descending inhibitory pathways. If your doc doesn’t know this, find a new one.
Just wanted to add something practical: if you’re using Miralax, mix it with water and drink it slowly over 10 minutes. Don’t chug it. It helps avoid the bloating that sometimes comes with it.
I also swear by keeping a small notebook in my purse-Bristol scale, pain level, food, stress. Even if I just scribble it. The pattern recognition is insane after a few weeks.
And for anyone thinking about ibodutant or Viome-hold off until it’s approved or validated. Don’t waste money on unproven tests. Stick to the basics: diet, stress, fiber, and tracking. That’s where the real progress happens.
Oh my god. I’ve been waiting for someone to actually write this without sugarcoating it.
So many people on here are like, "just eat more fiber!" or "try yoga!" Like, no. I’ve tried every fad. I’ve spent $2000 on probiotics that did nothing. I’ve cried in bathroom stalls at work. I’ve missed three weddings because I was too scared to leave the house.
And then I found out that loperamide isn’t a villain-it’s a tool. Like a fire extinguisher. You don’t use it every day. But when the house is burning? You grab it.
Also, if your doctor says "it’s stress," tell them to read the Rome IV guidelines. I did. They shut up.
Thank you. Finally. Someone who gets it.
OMG I’m so glad someone posted this because I’ve been so alone in this. I just had a flare and I was crying in the bathroom and I thought I was going crazy. I’ve been on this diet for 3 months and I still have bad days. Is it ever going to get better? I just want to eat a burrito without panic. 😭
From India, I’ve seen too many people blame IBS on "Western diets." But the truth? It’s not about food origin-it’s about gut sensitivity. We have high-FODMAP foods here too: lentils, onions, mangoes. The low FODMAP diet works because it’s science, not culture.
And yes, stress hits harder here. Family pressure, work hours, no mental health support. But tracking helped me. I started writing down what I ate and how I felt. Took me 6 weeks to see the pattern. Now I know: no coffee before 10am. No spicy food after 7pm. Small changes. Big results.
Also, psyllium works. Even here. I buy it online. It’s cheaper than your local "gut health" supplements.
Look, I’ve had IBS since I was 16. I’ve tried everything. Keto. Paleo. Gluten-free. Vegan. Nothing worked until I found the FODMAP diet. And guess what? It’s not that hard. You just need to stop being lazy and track your sh*t.
And no, you don’t need a dietitian. I did it on Reddit and YouTube. Took me 4 months. Now I eat pizza once a week and I’m fine. IBS-M isn’t a death sentence. It’s a puzzle. And you’re the only one who can solve it.
Also, loperamide is fine if you use it right. I take it on Fridays before going out. No shame. My gut doesn’t care what you think.
How can you Americans be so obsessed with pills and apps? In India, we’ve been treating this for centuries with ginger tea, jeera water, and walking after meals. No fancy science needed. You people are too dependent on technology. Your gut is weak because you sit all day and eat processed garbage.
Stop buying Miralax. Boil some cumin seeds. Drink it warm. Your body will thank you. And stop blaming stress-your lifestyle is the problem. Get up. Move. Eat real food. That’s it.
Bro, IBS-M is just your body saying "I’m tired of your nonsense." You eat junk, stress out, sleep 4 hours, then wonder why your butt is in revolt? 🤡
Try this: drink water before coffee. Walk 10 min after meals. Sleep like your life depends on it. No apps. No pills. Just basic human stuff.
Also, peppermint oil? Yes. Loperamide? Only if you’re about to board a flight. But don’t act like you’re some hero for taking it. We all know you’re just trying to survive your job.
PS: IBS-M doesn’t turn into cancer. Stop Googling at 3am. 😴