Why Managing Multiple Pharmacies and Prescribers Is a Safety Issue for Seniors
Seniors often take 5 to 10 medications at once. When those prescriptions come from different doctors and get filled at different pharmacies, the risk of dangerous interactions, duplicate drugs, or wrong dosages jumps sharply. Without a central system to track everything, a senior could end up with two blood thinners from two different prescribers-both approved, both legal, but deadly together. This isn’t rare. Studies show that 1 in 6 seniors on multiple medications experience a preventable error because their care is scattered across pharmacies and prescribers.
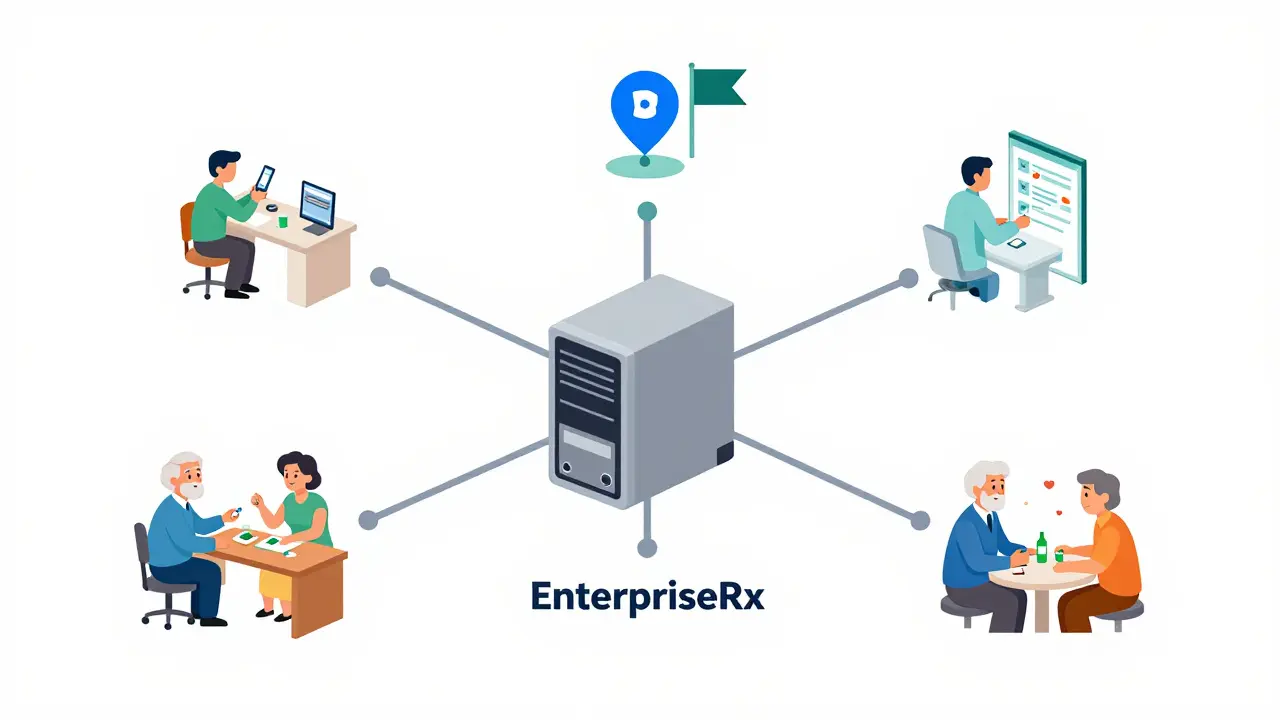
The fix isn’t more paperwork. It’s better systems. Centralized pharmacy management software connects every location, every prescriber, and every patient record in real time. It doesn’t just make things easier-it saves lives.
How Centralized Systems Prevent Medication Errors
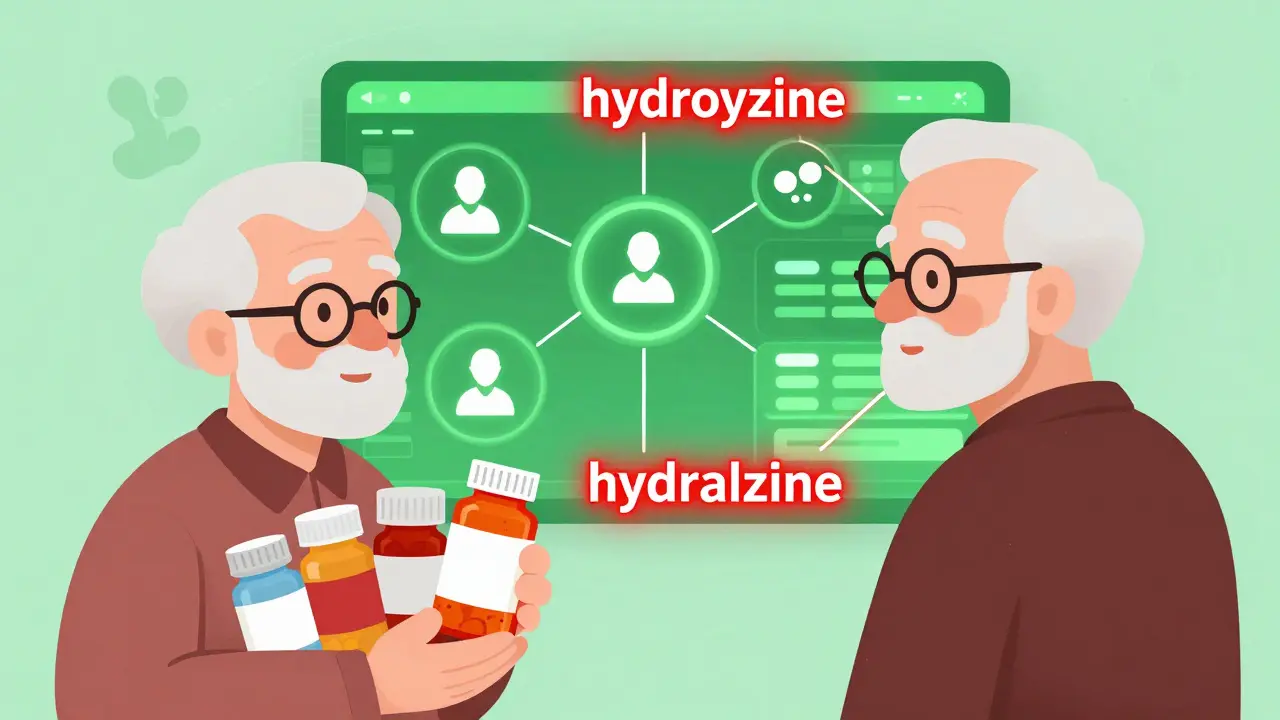
At the heart of safe multi-pharmacy management is a single, unified drug database. Every pharmacy in the network uses the same names, strengths, and NDC codes for every medication. No more confusion between "ibuprofen 200 mg" and "Advil 200 mg." No more mix-ups between similar-sounding drugs like hydroxyzine and hydralazine.
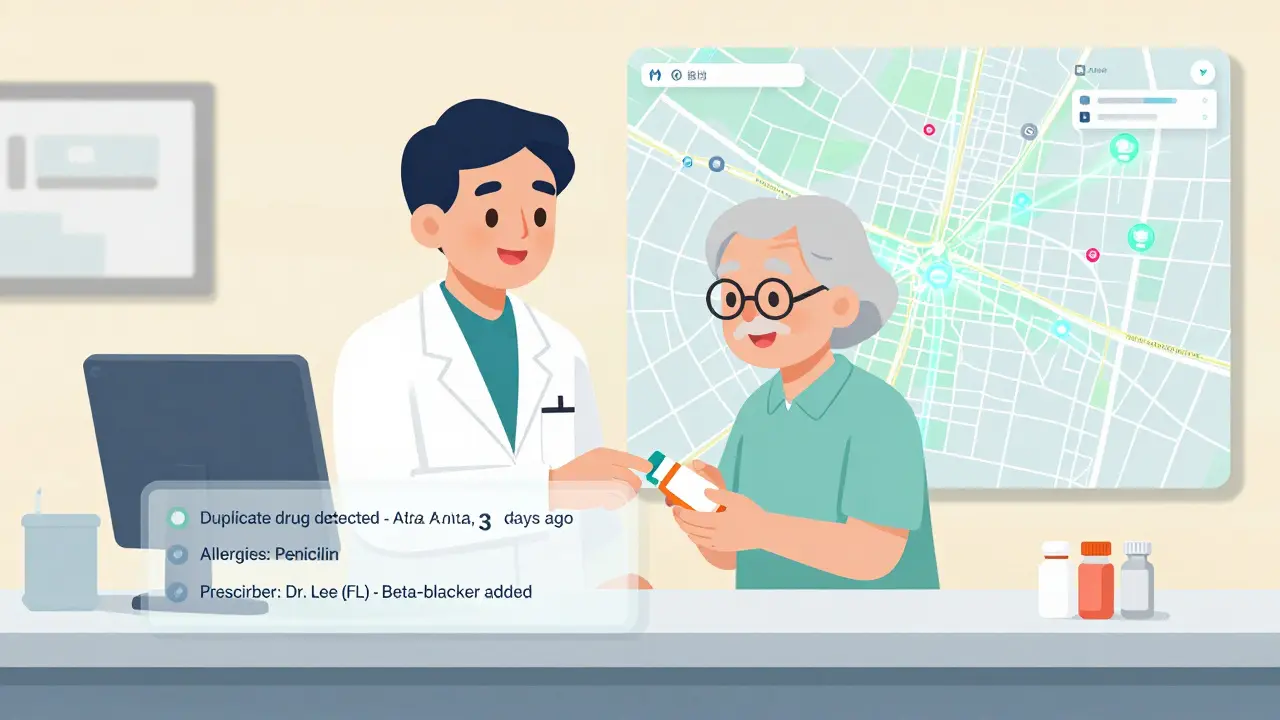
Without this standardization, errors occur in 1.3% of prescriptions across multiple locations. That might sound small, but for a chain serving 10,000 seniors monthly, that’s 130 preventable mistakes every month. Centralized systems like EnterpriseRx and PrimeRx eliminate that risk by locking in universal drug files. When a pharmacist in Chicago fills a prescription, the system instantly checks if the same drug was filled last week in Atlanta-and flags duplicates before the bottle is handed out.
These systems also track all prescribers linked to a patient. If a cardiologist in Florida prescribes a new beta-blocker, the system alerts every other pharmacy and prescriber in the network. No more hidden prescriptions. No more gaps.
Key Features That Make a Difference
Not all pharmacy software is built the same. Here’s what actually works for safety:
- Real-time patient profiles-Every pharmacy sees the same active med list, allergies, and past reactions. No more guessing.
- Automated drug interaction checks-The system runs 200+ interaction rules every time a new script comes in, even across prescribers.
- Inventory balancing-If one location runs low on a critical drug, the system suggests transfers from another store, avoiding delays for seniors who can’t wait.
- Watchdog monitoring-Systems like Datascan’s AI Watchdog 2.0 scan for odd patterns: a patient picking up opioids from three different locations in one week? It flags it automatically.
- Prescription transfer tools-Seniors can pick up meds at any location in the chain. No more driving across town because their usual pharmacy is closed.
These aren’t nice-to-haves. They’re the baseline for safe care. A 2023 study found chains using all five features saw a 41% drop in medication errors within six months.
Top Systems Compared: What Works Best
| System | Best For | Uptime | Cost per Location/Month | Key Safety Feature |
|---|---|---|---|---|
| EnterpriseRx | Large chains with 10+ locations | 99.98% | $325-$450 | Real-time prescriber alerts via Epic EHR integration |
| PrimeRx Pro | Pharmacies focused on patient convenience | 99.98% | $310-$400 | Seamless pickup location switching for patients |
| Datascan Central Store | Chains needing advanced monitoring | 99.99% | $290-$380 | AI Watchdog 2.0 for detecting prescription diversion |
| DocStation | Pharmacies offering clinical services | 99.97% | $340-$420 | Integrated billing for vaccines and chronic care visits |
| PharmacyOne Chain | Small chains on a budget | 99.95% | $299 | Basic inventory sync and shared patient records |
EnterpriseRx leads in clinical safety because it talks directly to hospital EHR systems. PrimeRx wins for convenience-seniors love being able to pick up meds at any location. Datascan’s AI Watchdog is unmatched for spotting abuse or diversion. DocStation helps pharmacies earn more by offering immunizations and medication therapy management. PharmacyOne is affordable but lacks advanced alerts.
How to Avoid Common Implementation Mistakes
Switching systems sounds simple. It’s not. Here’s what goes wrong-and how to fix it:
- Trying to migrate all data at once-Don’t move 5,000 patient records overnight. Do it in batches. One location at a time. A 2023 survey found 27% of chains had prescription errors during full migration because old and new systems clashed.
- Skipping staff training-Pharmacists need 24 hours of training. Technicians need 16. Chains that used vendor-certified trainers saw 12% higher adoption than those training internally.
- Letting local pharmacies make all clinical decisions-Centralized doesn’t mean robotic. But if every location ignores the system’s warnings, you lose the safety net. Set rules: if the system flags a duplicate, the pharmacist must document why they’re overriding it.
- Ignoring prescriber communication-The system can’t fix errors if doctors aren’t using it. Partner with local clinics. Offer free training. Make it easy for them to update med lists in real time.
Successful chains use the "hub-and-spoke" model: one central office handles drug files, pricing, and compliance. Each pharmacy keeps control over clinical judgment. That balance cut errors by 38% in a UC study.
Regulatory Pressures Are Making This Mandatory
It’s not just about safety anymore. It’s about compliance. Medicare Part D now requires multi-location pharmacies to prove they track prescription errors across all sites. CMS won’t pay you if you can’t show it.
By 2025, all systems must support FHIR APIs for seamless data sharing with EHRs. Right now, 63% of current software can’t do it without a $200,000+ upgrade. If you’re still using standalone software, you’re already behind.
The Pharmacy Quality Alliance predicts that by 2027, any pharmacy chain with three or more locations will be legally required to use a centralized system. Waiting isn’t an option. It’s a liability.
What’s Next: AI and Blockchain Are Changing the Game
The next wave isn’t just about connecting systems-it’s about predicting danger.
Datascan’s AI Watchdog 2.0, launched in January 2024, already identifies potential opioid diversion with 92.4% accuracy by spotting patterns across locations. Imagine a system that knows a senior’s refill pattern and alerts you if they suddenly start getting prescriptions from three new prescribers in a month.
Blockchain pilots are testing tamper-proof digital prescriptions. One trial reduced fraud by 67% in multi-location chains. No more forged scripts. No more stolen pills.
These aren’t sci-fi ideas. They’re rolling out now. The question isn’t if you’ll adopt them-it’s when.
Final Checklist for Safe Multi-Pharmacy Management
- ✅ Use a system with universal drug files and NDC standardization
- ✅ Ensure real-time patient profiles are visible at every location
- ✅ Enable automated interaction checks and duplicate alerts
- ✅ Implement a Watchdog-style monitoring tool for controlled substances
- ✅ Train all staff-pharmacists and techs-with certified vendors
- ✅ Use the hub-and-spoke model: central control, local judgment
- ✅ Verify prescriber integration with EHR systems
- ✅ Plan for FHIR API compliance by 2025
- ✅ Track error rates monthly-and reduce them
Frequently Asked Questions
Can I use one pharmacy system for both my retail and mail-order locations?
Yes, but only if the system supports both retail and mail-order workflows. EnterpriseRx and PrimeRx Pro handle both. Systems designed only for retail locations won’t process bulk mail-order prescriptions correctly. Make sure the software you choose has a dedicated mail-order module with automated refill scheduling and shipping integration.
How do I make sure prescribers actually use the system?
Don’t wait for them to come to you. Reach out to local clinics and hospitals. Offer free training sessions. Provide easy-to-use portals where prescribers can update med lists in real time. Some systems, like EnterpriseRx, now integrate directly with Epic and Cerner, so doctors see your pharmacy’s alerts inside their own EHR. That’s the gold standard.
What if my senior patients don’t want to switch pharmacies?
That’s why seamless transfer features matter. With systems like PrimeRx, patients can designate any location in your chain as their preferred pickup spot. They don’t need to change where they go-they just get more flexibility. Emphasize convenience, not disruption. Seniors care about ease, not software.
Is cloud-based software safe for sensitive patient data?
Yes-when it’s done right. All top systems use AES-256 encryption and FIDO2 security keys for access. They’re more secure than most local servers, which often lack updates and backups. Look for systems with 99.99% uptime and HIPAA-compliant data centers. Ask for third-party audit reports. If they won’t show them, walk away.
How long does it take to implement a new system?
For a chain with 5-10 locations, expect 8-12 weeks. Larger chains may take 4-6 months. The biggest delays come from data migration. Don’t rush it. Test with a small group of patients first. Validate 100% of active med lists before going live. A slow rollout with no errors beats a fast one with 14% of records wrong.
Can small chains with only 3 locations afford this?
Yes. PharmacyOne Chain starts at $299 per location monthly. That’s less than $9,000 a year for three locations. Compare that to the cost of one preventable medication error: potential lawsuits, lost Medicare reimbursements, and damaged reputation. The ROI isn’t just financial-it’s ethical.
What happens if the system goes down?
Top systems have 99.98%+ uptime and offline modes. When the network fails, pharmacies can still fill prescriptions using cached data. But they can’t override safety alerts without logging into the system later. Every offline fill must be reviewed within 24 hours. Make sure your vendor has a clear disaster recovery plan-and test it twice a year.