Every year, over 1.5 million people in the U.S. suffer preventable harm from medication errors. Many of these mistakes happen because someone didn’t stop to double-check the name, strength, or dosage form of a drug before giving it. It’s not always a mistake by a doctor or pharmacist-it’s often a quick glance, a misread label, or a tired moment when the brain skips a step. But checking medication details isn’t just a formality. It’s a life-or-death habit.
Why Checking Medication Details Matters
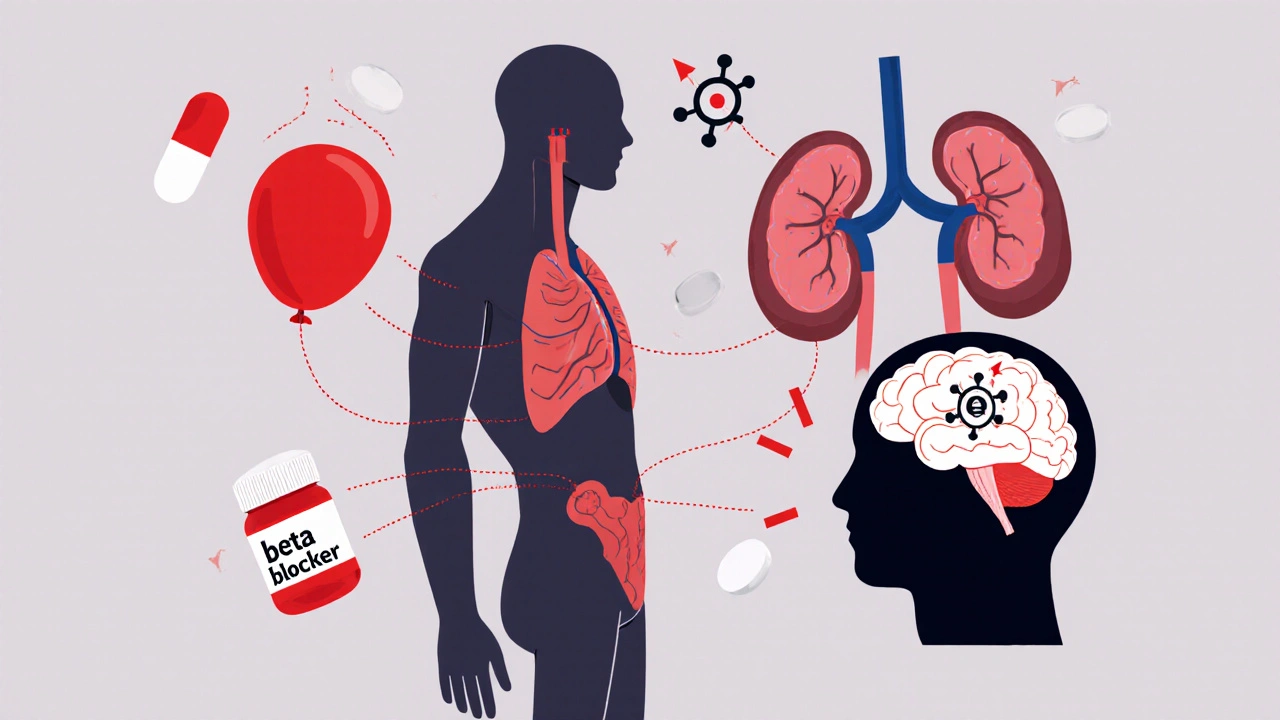
Medication errors aren’t rare. They’re common enough to kill about 7,000 people each year in U.S. hospitals alone. The biggest culprits? Confusing one drug for another because the names sound alike-like prednisone and prednisolone. Or misreading a strength: 10 mg instead of 100 mg. Or giving a pill meant to be swallowed when it was supposed to be applied to the skin. These aren’t hypothetical risks. They’ve caused real deaths.One nurse in a Reddit thread described how she caught a 100-fold overdose because she noticed the heparin vial said 5,000 units/mL, but the electronic order said 50 units/mL. She didn’t assume the system was right. She checked the label. That’s the kind of habit that saves lives.
Three Things to Check Every Time
There are three non-negotiable details you must verify every single time you handle a medication: the name, the strength, and the dosage form. Missing any one of them increases your risk.- Drug name: Is it spelled correctly? Is it the full name? Avoid abbreviations like “MS” (could mean morphine sulfate or magnesium sulfate) or “U” for units (which looks like “0”). Always write out “unit” and “mcg.”
- Strength: Is the number correct? Is the unit clear? Is it 5 mg or 50 mg? Is it 0.1 mg/mL or 1:10,000? Never rely on ratios for injectables-they’re too easy to misread. Convert them to decimals: 1:10,000 epinephrine = 0.1 mg/mL.
- Dosage form: Is it a tablet, capsule, liquid, patch, inhaler, or injection? Giving a pill meant for oral use as an injection can be fatal. Always confirm the form matches the route of administration.
The Institute for Safe Medication Practices (ISMP) found that just adding a space between the number and unit-writing 10 mg instead of 10mg-reduces errors by 12%. Why? Because 10mg can be misread as 100 mg if the “m” is smudged. That tiny space makes a huge difference.
How to Verify Medications at Each Step
Verification isn’t a one-time check. It’s a process that happens three times:- When you receive the order: Look at the prescription or electronic order. Does it include the full drug name, strength with units, dosage form, route, and frequency? If any part is missing, stop. Ask for clarification. Don’t guess.
- When you prepare the medication: Take the medication out of the container. Compare the label on the bottle or package to the order. Read the name out loud. Say the strength out loud. Confirm the form. If it’s a liquid, check the concentration. If it’s a tablet, check the imprint code. Don’t rely on color or shape alone-those can change between manufacturers.
- When you administer it: Before you give it to the patient, check again. Use the “read-back” method: say the drug name, strength, and dosage form out loud to yourself or to a colleague. Then confirm the patient’s identity. If something feels off, pause. It’s better to be late than wrong.
At Mayo Clinic, implementing a “four-eyes” rule-where two people verify high-risk medications like insulin or heparin-cut errors by 94% over 18 months. That’s not an exaggeration. It’s a documented result.

Common Traps and How to Avoid Them
Even experienced professionals get tripped up. Here are the most frequent mistakes-and how to dodge them:- Insulin confusion: Insulin comes in different strengths (U-100, U-500). A single mistake can cause a coma. Always double-check the vial label. Never assume. Use a magnifying glass if the print is small.
- “U” for units: Writing “U” looks like a “0” or a “4.” Always write out “unit.”
- Leading zeros: Write 0.5 mg, not .5 mg. A missing zero can make a dose ten times bigger.
- Tall Man lettering: For look-alike drugs, use capital letters to highlight differences: predniSONE vs. predniSOLONE. This reduces confusion by 76%.
- Abbreviations: Avoid “QD” (daily), “QID” (four times a day), or “cc.” Use “daily,” “four times daily,” or “mL.”
A 2024 survey of 850 pharmacy technicians found that 12% still saw “MS” used for magnesium sulfate in emergency rooms. That’s dangerous. Magnesium sulfate can stop seizures. Morphine sulfate can stop breathing. One letter, one mistake, one life lost.
Technology Helps-but Doesn’t Replace Human Checks
Electronic health records and barcode scanners are powerful tools. Hospitals using barcode medication administration (BCMA) cut dispensing errors by 83%. Systems like Epic and Cerner can flag look-alike names and calculate correct doses automatically.But here’s the catch: people start trusting the machine too much. A 2020 study by The Joint Commission found that 18% of errors happened because clinicians ignored a warning because the system said “approved.” That’s called automation bias. The screen says it’s fine? Then you don’t look again. That’s when things go wrong.
Technology should support you, not replace your brain. Always verify the physical label against the screen. Always read the name, strength, and form yourself-even if the computer says it’s right.
What to Do If You’re Unsure
If you’re confused, pause. Don’t rush. Ask someone. Call the pharmacy. Check a trusted reference like the FDA’s Drug Shortage List or the ISMP’s Medication Safety Alerts. There’s no shame in asking. There’s only shame in guessing.One nurse shared how she once held a vial of insulin and thought, “This doesn’t feel right.” She didn’t know why. She called the pharmacy. Turns out, the order was for U-100, but the pharmacy sent U-500. She caught it before the patient got it. That’s the power of trusting your gut.

Training and Culture Make the Difference
Hospitals that require four hours of initial medication safety training and quarterly 30-minute refreshers cut errors by 63%. Why? Because repetition builds habit. Because people learn to pause. Because safety becomes part of the culture-not just a rule on a poster.It’s not about blame. It’s about systems. The goal isn’t to find who messed up. It’s to make sure no one ever has to make that mistake again.
What’s Changing in 2025?
The FDA is pushing for digital drug labels that can be read by machines-think QR codes on pill bottles that link to full safety info. AI tools are being tested to scan medication labels and spot errors using image recognition. Google Health’s pilot program got 99.2% accuracy in identifying mismatches.But these tools aren’t ready for prime time. They still need human validation. Until then, the most reliable tool you have is your eyes, your brain, and the discipline to check-every time.
Final Reminder: Slow Down to Stay Safe
Medication safety isn’t about being perfect. It’s about being consistent. You don’t need to memorize every drug. You just need to slow down long enough to read the name, the number, and the form. Three checks. Every time. No exceptions.It’s not about trust. It’s about verification. Because when it comes to medicine, the difference between a dose that heals and a dose that harms is often just a decimal point, a missing space, or a single letter.
What should I do if a medication label looks different from the prescription?
Stop. Don’t give it. Compare the name, strength, and dosage form on the label with the original order. If they don’t match exactly, contact the prescribing provider or pharmacy. Never assume the label is correct just because it came from the pharmacy. Always verify.
Can I rely on electronic health records to catch medication errors?
Electronic systems can help flag potential errors, but they’re not foolproof. Studies show that 18% of errors happen because clinicians ignore alerts due to “alert fatigue.” Always cross-check the physical medication label with the screen. Technology supports you-it doesn’t replace your responsibility to verify.
Why is spacing important in medication dosing (e.g., 10 mg vs. 10mg)?
Spacing prevents misreading. Writing “10mg” without a space can be mistaken for “100 mg” if the “m” is unclear or smudged. The Institute for Safe Medication Practices found that adding a space reduces this type of error by 12%. Always write the number, space, then unit: “10 mg,” “5 mL,” “0.5 mcg.”
What’s the safest way to verify insulin?
Insulin errors are among the most dangerous. Always check the vial label for the concentration (U-100, U-500). Never assume. Use a magnifying glass if needed. Verify the strength against the prescription. Use the “read-back” method: say aloud, “This is U-100 insulin, 10 units.” Double-check with another person if possible. Never use abbreviations like “U” for units-write “unit.”
Are abbreviations like “MS” or “QD” still used, and are they dangerous?
Yes, and they’re extremely dangerous. “MS” can mean morphine sulfate or magnesium sulfate-two drugs with opposite effects. “QD” (daily) can be mistaken for “QID” (four times daily). These abbreviations are banned by safety organizations like ISMP and The Joint Commission. Always write out “morphine sulfate,” “magnesium sulfate,” “daily,” or “four times daily.”
What should I do if I notice a pattern of errors in my workplace?
Report it. Don’t stay silent. Document the specific errors-what drug, what mistake, how often. Bring it to your supervisor or safety officer. Many hospitals have anonymous reporting systems. If systems are broken, fixing them requires data. Your observation could prevent a tragedy.


I used to think I was too careful until I saw a coworker hand a patient insulin labeled U-500 thinking it was U-100. She didn’t check the vial-just trusted the barcode. That moment changed everything. Now I read every label out loud, even at 3 a.m. No exceptions. That space between 10 and mg? I now treat it like a seatbelt. Tiny thing. Huge consequences.
And yes, I still use a magnifying glass for insulin. No shame in needing it.
Bro this is literally life or death 😭 I once saw a nurse give someone a pill that was supposed to be a patch-like, straight up swallowed it. Guy ended up in ICU. We all thought it was a joke at first. It wasn’t. 🙏 Always check. Always. Even if you’re tired. Even if you’ve done it a thousand times. That’s the moment it slips.
Also, tall man lettering? YES. predniSONE vs predniSOLONE. It’s like seeing the difference between ‘bat’ and ‘bait.’ One letter, whole different animal.
The real issue isn’t human error-it’s systemic failure. We’ve built a culture where speed is valued over safety, and then we act shocked when someone dies because a label was misread. The four-eyes rule works because it forces accountability. But why does it take a near-fatal mistake to implement basic checks? Why are we still using ‘U’ for units in 2025? This isn’t about training. It’s about power. The system rewards efficiency, not vigilance. And until we flip that script, no amount of mnemonics or spacing will save lives.
We don’t need more rules. We need to stop pretending this is a personal responsibility issue. It’s a structural one.
Every single time you handle a medication, you must verify the name, strength, and dosage form. No shortcuts. No assumptions. No exceptions. This is not optional. This is not a suggestion. This is a non-negotiable standard of care. If you skip one step, you are putting a human life at risk. Period.
The Institute for Safe Medication Practices has documented this repeatedly. The data is clear. The consequences are fatal. If your workplace doesn’t enforce this, you have a duty to escalate it. Silence is complicity.
I remember being a new nurse and feeling so overwhelmed-I thought I’d forget something. Then I started saying the drug name out loud while holding the vial. ‘This is insulin glargine, 10 units, U-100.’ Just saying it made me pause. And that pause? That’s what saved me more than once.
It’s not about being perfect. It’s about being present. And if you’re too tired to do that? Don’t give meds. Ask for help. You’re not weak for pausing. You’re the reason someone goes home.
okay but like… what if you’re just really tired and your eyes are blurry and the label is tiny and you’re on your 12th shift this week?? 😩 i’ve been there. i held a vial and thought ‘is this… is this 500 or 100??’ and i just cried a little and called the pharmacy. no one judged me. they said ‘thank you.’
so yeah. if you’re unsure? ask. your hands are holding someone’s life. it’s okay to be scared. just don’t be silent.
They don’t want you to know this but the FDA and Big Pharma are pushing these ‘safety’ rules to make you dependent on their systems. They want you to trust the machine. But the real danger? The vials are pre-labeled with microchips that track your every move. That’s why they’re pushing QR codes and AI scanners. They’re not protecting you-they’re profiling you.
And don’t get me started on ‘tall man lettering.’ That’s just another way to confuse you. PredniSONE? Sounds like a brand name. It’s mind control. Wake up.
Just trust your gut. And never trust a label. Ever.
Back home in India, we don’t have barcode scanners or Epic systems. We have handwritten scripts, dim lights, and nurses who memorize 50+ drug names. But we still check. Because we know: one mistake, one life gone.
Spacing? We write ‘10 mg’ with a pen that runs out of ink. We lean in. We squint. We ask. No fancy tech. Just care.
This isn’t about American tech. It’s about human attention. And that’s free.
Let’s be real-this whole ‘three checks’ thing is just a distraction. The real problem? The pharmaceutical industry controls the labels. They design drugs with names that sound alike on purpose. Prednisone and prednisolone? Same company. Same profit margin. Different side effects.
And the ‘four-eyes rule’? That’s not safety. That’s liability insurance. They want you to feel safe so you don’t sue them when the AI misreads the QR code and gives someone 1000 units of insulin.
They’re not here to protect you. They’re here to monetize your fear.
And don’t even get me started on ‘U’ for units. That’s not a typo. It’s a trap.