Most people with chronic insomnia are told to sleep better-turn off the lights, avoid caffeine after noon, keep the room cool. But if you’ve been struggling with sleep for months or years, you know that advice doesn’t fix anything. That’s because sleep hygiene isn’t a cure. It’s a side note. And relying on it alone is like trying to fix a broken engine by washing the outside of your car.
What Chronic Insomnia Really Is
Chronic insomnia isn’t just having a bad night’s sleep. It’s a medical condition defined by trouble falling asleep, staying asleep, or waking up too early-happening at least three nights a week for three months or longer. The American Academy of Sleep Medicine says this isn’t normal stress or jet lag. It’s a persistent disruption in your brain’s sleep-wake system.
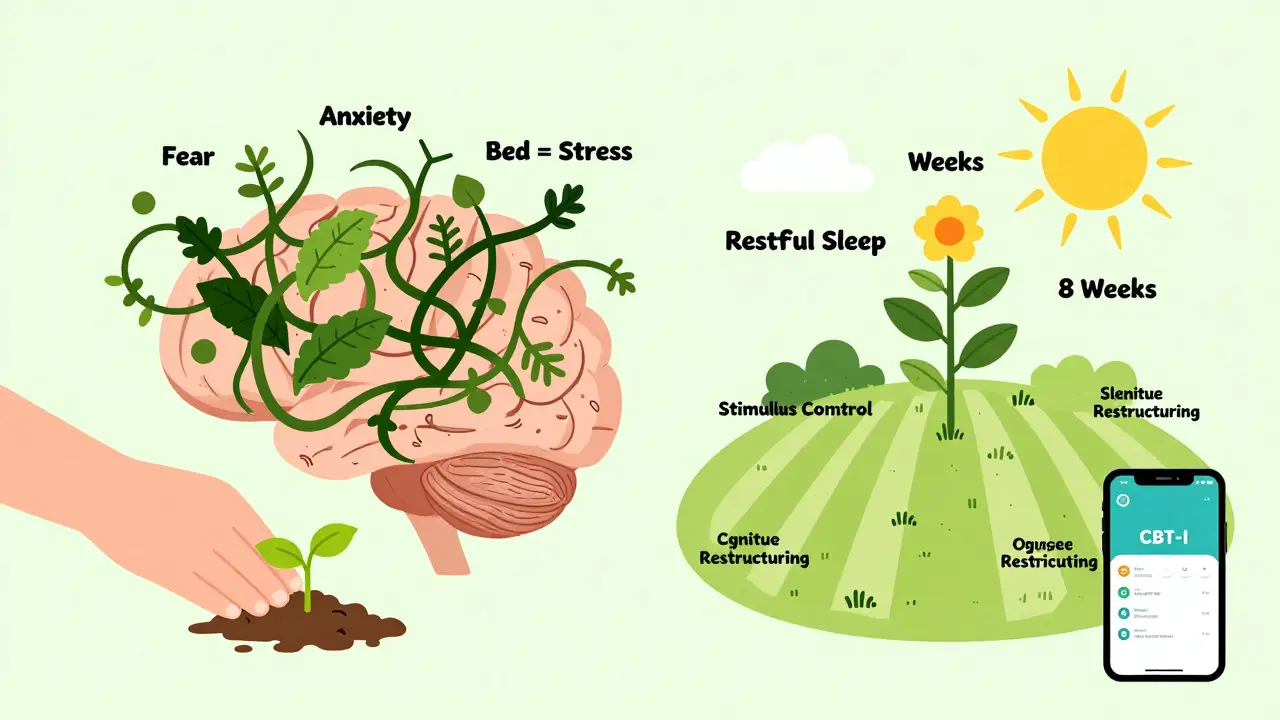
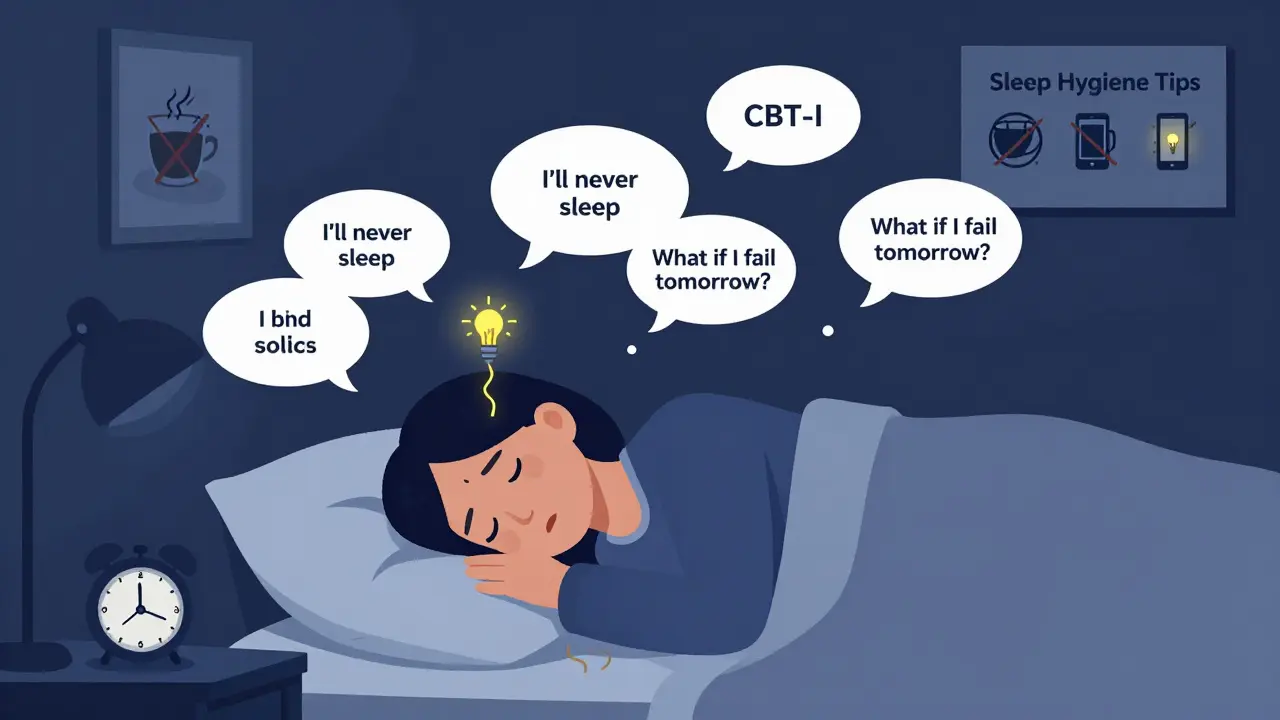
People with chronic insomnia often feel exhausted during the day, anxious about sleep, and trapped in a cycle: they lie awake, get frustrated, try harder to sleep, and end up even more alert. Their bodies start associating the bed with stress instead of rest. This isn’t laziness. It’s not a lack of willpower. It’s a learned pattern that’s been reinforced over time.
Why Sleep Hygiene Doesn’t Work for Chronic Insomnia
Sleep hygiene-things like avoiding screens before bed, keeping your room dark, not drinking coffee after 2 p.m.-sounds logical. And it helps a little if you’re just having occasional trouble. But for chronic insomnia? The evidence is clear: it’s not enough.
The American Academy of Sleep Medicine rates sleep hygiene as having only moderate evidence of effectiveness. That means it might help someone who’s sleeping poorly because they’re scrolling through TikTok at 2 a.m. But for someone who’s been awake for hours every night for six months? Sleep hygiene alone changes nothing.
Dr. Jack D. Edinger, one of the leading researchers in insomnia, says bluntly: “Sleep hygiene education alone is minimally effective for chronic insomnia and should not be offered as standalone treatment.” The Health.mil Patient Guide echoes this: “Do not use sleep hygiene as a standalone treatment for chronic insomnia.”
Why? Because chronic insomnia isn’t caused by bad habits. It’s caused by thoughts, fears, and behaviors that have become automatic. You’re not lying awake because your room is too warm. You’re lying awake because you’re terrified you won’t sleep-and that fear keeps your brain wired.
CBT-I: The Only Treatment That Changes the Brain’s Sleep Pattern
The only treatment backed by strong, long-term evidence for chronic insomnia is Cognitive Behavioral Therapy for Insomnia, or CBT-I. It’s not a pill. It’s not a gadget. It’s a structured program that rewires how you think about sleep-and how you behave in bed.
The American College of Physicians, the American Academy of Sleep Medicine, and the National Institutes of Health all say CBT-I should be the first treatment for chronic insomnia. Not after medication. Not as a last resort. First.
Studies show 70-80% of people who complete CBT-I see real, lasting improvements. That’s better than any sleeping pill. And unlike pills, the benefits don’t vanish when you stop. In fact, they often get stronger.
The Five Core Parts of CBT-I
CBT-I isn’t one thing. It’s five techniques, all working together. A trained therapist walks you through them over 6-8 weekly sessions, though some digital programs deliver them in as few as two.
1. Stimulus Control Therapy
This is the most counterintuitive part. You’re told: Get out of bed if you’re not asleep in 15-20 minutes.
Most people with chronic insomnia stay in bed, tossing and turning, hoping sleep will come. But your brain learns: bed = anxiety = wakefulness.
Stimulus control breaks that link. Only go to bed when sleepy. Get up if you’re not asleep after 20 minutes. Go do something quiet in dim light-read a book, listen to calm music-then return to bed only when sleepy again. And no matter how little you slept, wake up at the same time every day, even on weekends.
One Reddit user wrote: “I thought this was ridiculous. But after two weeks, I stopped dreading bedtime. I finally associated my bed with sleep.”
2. Sleep Restriction
This sounds brutal. You’re told to spend less time in bed-not more.
If you’re only sleeping 5 hours a night but lying in bed for 8, your sleep efficiency is low. Sleep restriction cuts your time in bed to match your actual sleep time. So if you’re sleeping 5 hours, you’re only allowed to be in bed for 5 hours. You go to bed later and wake up earlier.
It’s exhausting at first. You’ll feel like a zombie. But that mild sleep deprivation increases your body’s drive to sleep. After a week or two, your sleep efficiency climbs. Then, you slowly add back 15 minutes of bed time every few days-until you’re sleeping 7 hours without lying awake for 3.
A 2020 meta-analysis found CBT-I reduced time to fall asleep by 18.2 minutes and nighttime wakefulness by 27.4 minutes. Medications? Only 12.1 and 15.8 minutes. And the medication gains disappeared after stopping. CBT-I’s improvements lasted a year later.
3. Cognitive Restructuring
This is where the real change happens. You start noticing the thoughts that keep you awake: “If I don’t sleep 8 hours, I’ll fail at work.” “I’m going to be a mess tomorrow.” “I’ll never get better.”
These aren’t just worries. They’re beliefs your brain treats as facts. Cognitive restructuring helps you challenge them.
For example: “Is it true that everyone needs 8 hours? Studies show most adults need 7-7.5. Even 6.5 is fine for some.” Or: “Have you ever been sleep-deprived and still functioned? You did. You’re not broken.”
A 2019 study in the Journal of Clinical Sleep Medicine found cognitive restructuring reduced sleep-related anxiety in 65% of patients. That’s not just feeling better. That’s breaking the fear cycle that keeps insomnia alive.
4. Relaxation Training
Chronic insomnia keeps your nervous system on high alert. Your body is stuck in “fight or flight.” Relaxation techniques-like diaphragmatic breathing, progressive muscle relaxation, or mindfulness-teach your body how to calm down.
It’s not about forcing sleep. It’s about lowering the internal noise so sleep can happen naturally.
5. Sleep Hygiene (The Right Way)
Sleep hygiene isn’t useless-it’s just not the main tool. In CBT-I, it’s used as a supporting player:
- Keep your bedroom at 65°F (18.3°C)-cool is better for sleep.
- Use blackout curtains or a sleep mask. Even small amounts of light disrupt melatonin.
- Use white noise to mask sudden sounds-door slams, traffic, snoring.
- Avoid caffeine after 2 p.m. (some people need to cut it off by noon).
- Limit alcohol to 1-2 drinks, finished at least 4 hours before bed. Alcohol may help you fall asleep but wrecks deep sleep later.
- Stop drinking fluids after 7 p.m. to avoid bathroom trips.
These aren’t rules to follow on their own. They’re tweaks to support the real work: changing how your brain responds to bed and sleep.

How Long Does CBT-I Take to Work?
It’s not instant. The first two weeks of sleep restriction are often the hardest. Many people report feeling worse before they feel better. That’s normal.
Most people start seeing improvement in 2-4 weeks. Full results take 8-12 weeks. The key is consistency. Missing sessions or skipping sleep restriction because you’re tired defeats the purpose.
One user on Patient.info said: “The sleep restriction part was brutal. I was falling asleep at my desk. But after week three, I slept 6.5 hours straight for the first time in years.”
What About Sleeping Pills?
Pills like zolpidem, eszopiclone, or suvorexant can help in the short term-say, after a major life stress or during travel. But they don’t fix the root problem. After 4-6 weeks, their effectiveness drops. And you can become dependent.
CBT-I has no risk of addiction. No grogginess. No memory issues. And the benefits last.
A 2020 review in Sleep Medicine Reviews found CBT-I outperformed medication on every measure: faster sleep onset, less nighttime wakefulness, better daytime function-and lasting results.
Can You Do CBT-I Online?
Yes. And it works.
Programs like Sleepio and SHUTi are FDA-cleared digital CBT-I platforms. A 2021 JAMA Internal Medicine trial found 50-60% of users reached remission (no more insomnia symptoms) after 6 weeks. Only 15-20% of the control group did.
Apps like Somryst are now prescribed by doctors. They track your sleep, adjust your schedule, and deliver CBT-I modules through your phone. One study showed 55.4% remission rates-comparable to in-person therapy.
But not all apps are equal. Look for ones that include all five components of CBT-I-not just sleep tracking or meditation. Check if they’re backed by peer-reviewed studies.
Why Isn’t Everyone Getting CBT-I?
Because it’s hard to access.
The U.S. has only 0.5 CBT-I-certified therapists per 100,000 people. In rural areas, 78% of counties have no sleep specialist at all. Insurance often covers only 3-4 sessions, even though 6-8 are recommended.
One Reddit user wrote: “My insurance only paid for 3 sessions. I couldn’t finish. I gave up.”
But digital CBT-I is changing that. It’s cheaper, scalable, and available 24/7. Companies like Pear Therapeutics are developing AI-driven versions that personalize the program based on your sleep data.
And it’s catching on: 37% of Fortune 500 companies now offer CBT-I through employee wellness programs. The digital CBT-I market is expected to hit $1.2 billion by 2027.
What’s Next for Insomnia Treatment?
Experts predict CBT-I will become the standard of care for 90% of chronic insomnia cases within the next decade. Sleep specialists are moving away from pills entirely, reserving them only for short-term crises.
Wearables like Fitbit are now integrating CBT-I principles into their sleep profiles, using 30+ nights of data to suggest personalized bedtimes. AI is being used to predict when someone is at risk of relapse and intervene before it happens.
Dr. Andrew Krystal, a leading sleep researcher, says: “CBT-I will become the standard of care for 90% of chronic insomnia cases within the next decade, with pharmacotherapy reserved for acute, short-term use only.”
How to Start CBT-I Today
1. Track your sleep for 7-14 days. Write down when you get in bed, when you fall asleep, when you wake up, and how many times you woke up. Use a notebook or a free app like Sleep Cycle or SleepScore.
2. Calculate your sleep efficiency: (Total sleep time / Time in bed) × 100. If it’s below 85%, you’re a candidate for sleep restriction.
3. Set a fixed wake-up time. No exceptions. Even on weekends. This is the most important rule.
4. Download a CBT-I app like Sleepio, SHUTi, or Somryst. Look for ones with published clinical trials.
5. Be patient. The first two weeks will be rough. Don’t quit. The breakthrough comes after the struggle.
6. Don’t use sleep hygiene alone. It’s a helper, not a cure.
Chronic insomnia isn’t your fault. It’s not weakness. It’s a brain habit. And like any habit, it can be unlearned-with the right tools.
CBT-I isn’t magic. But it’s the only thing that works long-term. And it’s waiting for you to try it.
Let’s be real-sleep hygiene is the placebo of the wellness industrial complex. You wash the outside of your car and call it maintenance? Bro, the engine’s rusted out and you’re polishing the hubcaps. CBT-I isn’t just ‘therapy’-it’s neuroplasticity warfare. Your brain learned to fear sleep. Now you unlearn it with behavioral conditioning, not lavender sprays and ‘no screens after 9.’
And yes, sleep restriction feels like being tortured by a sleep scientist. You’re exhausted. You’re irritable. You’re questioning your life choices. But that’s the point. You’re rebuilding the neural pathway from ‘bed = panic’ to ‘bed = sleep.’ It’s not magic. It’s neuroscience. And it works.
70-80% success rate? That’s not a stat. That’s a revolution. Pills? Temporary Band-Aids with a side of dependency. CBT-I? You walk away with a rewired brain and zero prescriptions. Who’s the real hack now?
I tried CBT-I through an app last year. The sleep restriction part almost broke me. I remember sitting at my desk at 3 p.m. with my head on the keyboard, crying because I couldn’t stay awake. But after week four, I slept 7 hours straight for the first time in five years. I didn’t believe it would work. I still don’t fully trust it. But I’m sleeping. And that’s enough.
CBT-I is the OG sleep hack 💪🔥 I was skeptical too until I did it. Now I sleep like a baby (and I’m 42). No pills. No weird gadgets. Just discipline + science. If you’re still doing ‘sleep hygiene’ like it’s a yoga pose… you’re wasting time. Go download Sleepio. Do the work. Your future self will hug you.
Okay but like… I tried CBT-I… and the therapist was so pushy?? Like I said I was tired and she said ‘you’re not tired, you’re avoiding sleep’ and I was like… I’ve been awake for 18 hours?? And then she made me track my sleep in a spreadsheet?? Like… why is this so intense?? I just wanted to sleep, not get a PhD in insomnia… 😭
Also I did the sleep restriction thing and I fell asleep at my dog’s vet appointment. I’m not proud. But I slept 6 hours straight after 3 weeks. So… maybe? I dunno. I’m still traumatized.
Let me tell you something sweet, buttercup-sleep hygiene is the glitter glue of insomnia treatment. Pretty, sparkly, and utterly useless when the whole damn thing’s falling apart. CBT-I? That’s the industrial epoxy. It doesn’t just stick-it bonds. It restructures. It rebuilds from the inside out.
And don’t even get me started on pills. You think zolpidem’s gonna save you? Nah. That’s just a one-way ticket to zombie mode and a $200 monthly habit. CBT-I? You get your brain back. No side effects. No withdrawal. Just quiet, deep, stolen-in-the-dead-of-night sleep. And that? That’s freedom.
People think sleep is about routines. Nah. It’s about rewiring. You’re not broken. You’re just stuck in a loop your brain wrote when you were stressed, scared, or just plain tired. Now you’re editing the script. And it’s beautiful.
CBT-I is overhyped. I’ve seen 30+ patients in my sleep clinic. Half of them dropped out after week two because they couldn’t handle sleep restriction. The other half? They improved, sure-but their sleep quality regressed within 6 months without ongoing coaching. Digital apps? They’re glorified chatbots with a fancy UI. Real CBT-I needs human feedback, not algorithmic nudges.
And let’s be honest: if you’re in a high-stress job, living in a noisy apartment, or raising kids, CBT-I is a luxury. You can’t ‘retrain your brain’ when you’re surviving. Pills aren’t perfect, but sometimes they’re the only thing keeping you functional.
CBT-I is the only evidence-based solution. Sleep hygiene is a myth for chronic cases. The data is overwhelming. Digital platforms like Sleepio have randomized trial validation. The only barrier is access. Insurance won’t cover it. Therapists are scarce. But the science is solid. Don’t confuse convenience with efficacy.
I followed the CBT-I protocol for 10 weeks. Fixed wake-up time. Sleep restriction. Stimulus control. It was brutal. But I slept through the night for the first time since 2019. I’m not saying it’s easy. But it’s the only thing that worked. And I didn’t need a therapist. The app did it. The science is real. Stop listening to the ‘just sleep better’ noise.
Wow. Just… wow. You people are so obsessed with ‘fixing’ sleep like it’s a broken appliance. What if the problem isn’t your brain? What if it’s your life? You’re stressed, overworked, lonely, and you think a 6-week app is going to fix that? You’re not treating insomnia-you’re treating symptoms of a broken society. And now you’re selling it as a self-help product. That’s not healing. That’s capitalism.
And you call it ‘evidence-based’? That’s just fancy words to make people feel better about paying $200 for an app while their boss demands 70-hour weeks. Wake up. Sleep isn’t the problem. Your life is.