Food-Drug Interaction Checker
Check if your medication interacts with food or beverages. Many common foods can reduce medication effectiveness or cause dangerous side effects.
Select a medication and food to see results
Many people don’t realize that what they eat can change how their medicine works-sometimes in dangerous ways. Taking a pill with your morning coffee or eating a grapefruit while on a statin might seem harmless, but these habits can make your medication less effective, increase side effects, or even cause life-threatening reactions. The truth is, food-drug interactions are one of the most common-but often overlooked-reasons people end up in the hospital because of their medications.
How Food Changes How Your Medicine Works
Food doesn’t just fill your stomach; it changes your body’s chemistry. When you eat, your digestive system kicks into gear. Your stomach acid increases, your blood flow shifts to your gut, and enzymes start breaking down nutrients. All of this can interfere with how your body absorbs, processes, or removes a medication.
There are three main ways food affects drugs:
- Pharmacokinetic interactions-These change how your body moves the drug around. For example, food can block absorption, speed it up, or slow it down.
- Pharmacodynamic interactions-These change how the drug acts in your body. A food might make a drug stronger or weaker at its target site.
- Physicochemical interactions-This is when food physically binds to the drug, like calcium in milk sticking to an antibiotic and carrying it out of your system before it can work.
One of the most common problems? Taking medicine with food when you’re supposed to take it on an empty stomach. Studies show 68% of patients don’t understand what “take on empty stomach” really means. It doesn’t mean “wait 10 minutes after your toast.” It means at least one hour before or two hours after eating. A 2022 study in JAMA Internal Medicine found that taking levothyroxine (a thyroid hormone) with breakfast cuts its effectiveness by 34%. That’s not a small difference-it can mean your thyroid stays under-treated, leading to fatigue, weight gain, and heart problems.
Top 5 Food-Drug Interactions You Need to Know
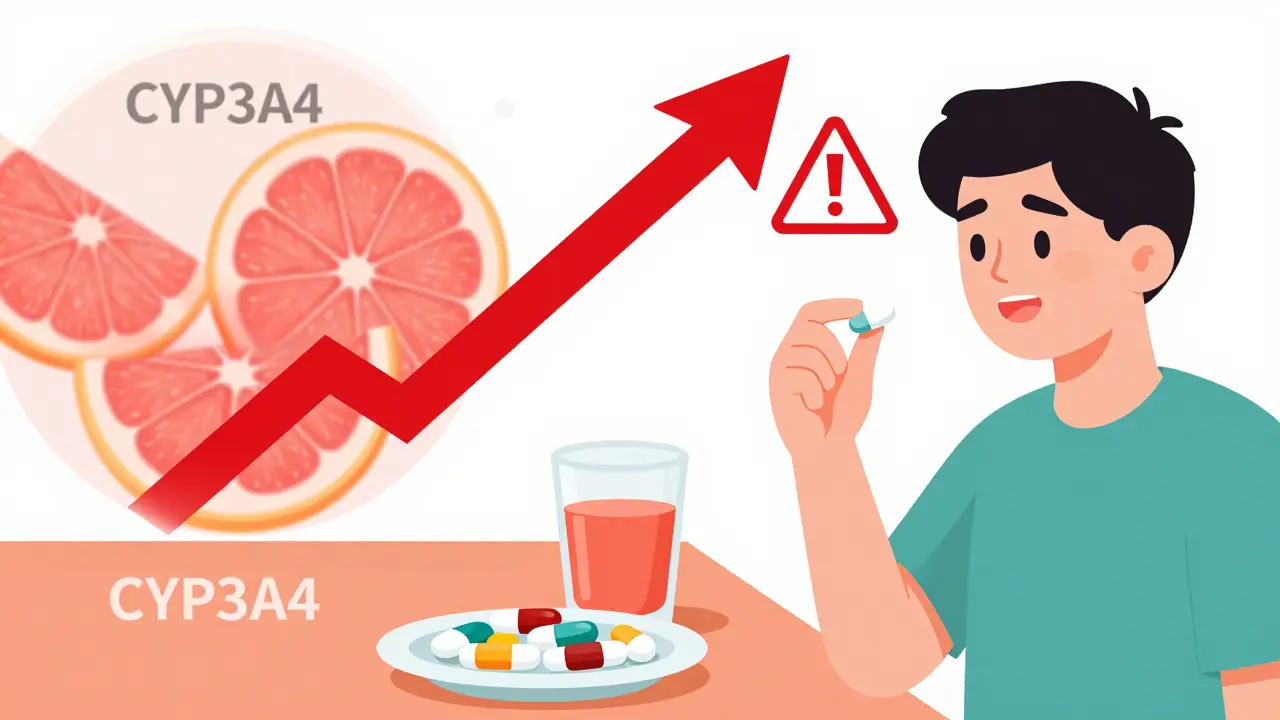
1. Grapefruit Juice and Statins
Grapefruit juice isn’t just sour-it’s powerful. It blocks an enzyme in your gut called CYP3A4, which normally breaks down certain drugs before they enter your bloodstream. When that enzyme is shut down, the drug builds up. With simvastatin (a cholesterol drug), grapefruit juice can increase blood levels by 330%. That’s not just a higher chance of side effects like muscle pain-it can lead to kidney failure. Even a single glass can have effects that last over 24 hours. Other drugs affected include some blood pressure pills, anti-anxiety meds, and transplant rejection drugs.
2. Dairy and Antibiotics
Calcium in milk, yogurt, and cheese binds tightly to antibiotics like tetracycline and ciprofloxacin. This creates a kind of chemical handcuff-your body can’t absorb the drug properly. Research from Parkview Medical Center shows this cuts absorption by up to 50%. That means the antibiotic might not reach the infection, letting it grow stronger. The fix? Wait at least two hours before or after eating dairy to take these antibiotics. For some, like doxycycline, even a glass of milk can ruin the dose.
3. Leafy Greens and Warfarin
If you’re on warfarin (a blood thinner), your vitamin K intake matters. Vitamin K helps your blood clot. Warfarin works by slowing that process. If you eat a big salad one day and no greens the next, your INR (a blood test that measures clotting time) swings wildly. That’s dangerous-too high, and you risk bleeding; too low, and you risk clots. Cooked spinach has 483 mcg of vitamin K per cup. A consistent intake within 10-15% daily variation is key. People who track their greens with a food diary have 28% fewer INR problems, according to the American Heart Association.
4. Alcohol and Painkillers
Alcohol and acetaminophen (Tylenol) is a risky combo. Both are processed by the liver. Together, they can overwhelm it, leading to liver damage-even if you’re taking the right dose. Alcohol also makes NSAIDs like ibuprofen more likely to cause stomach ulcers. A Mayo Clinic study found that taking ibuprofen without food causes ulcers in 15% of users. With food? That drops to 4%. But alcohol? It cancels out the protection. Combine alcohol with opioids or sedatives? That’s a recipe for slowed breathing or coma.
5. High-Fat Meals and Some Antifungals
Not all interactions are bad. Some drugs actually work better with food. Griseofulvin (used for fungal infections) and diazepam (Valium) absorb 25-35% more when taken with a high-fat meal. Fat helps these drugs dissolve and enter your bloodstream. If you take them on an empty stomach, you might not get the full benefit. Always check the label: if it says “take with food,” don’t skip the cheese or avocado.

Why Some Medications Are More Sensitive Than Others
Not all drugs are equally affected. Some are like delicate instruments, easily thrown off by food. Others? They barely notice what you eat.
Antibiotics have the most food interactions. Fluoroquinolones like ciprofloxacin lose up to 90% of their power when taken with calcium. But amoxicillin? It’s mostly unaffected. Why? Because some drugs are absorbed in the upper gut, where food quickly moves in. Others are absorbed lower down, where food has less impact.
Cardiovascular drugs show big differences too. Warfarin has 17 known food interactions. Apixaban (Eliquis)? Only 3. That’s why doctors often switch patients from warfarin to newer blood thinners-it’s easier to manage. Proton pump inhibitors like omeprazole need to be taken 30-60 minutes before meals to block stomach acid. But famotidine? It works fine with or without food.
MAO inhibitors (used for depression) are the most restrictive. Foods like aged cheese, cured meats, and fermented soy can trigger a sudden, deadly spike in blood pressure. Tyramine in these foods can raise blood pressure by 50-100 points in minutes. That’s why patients on these drugs get detailed dietary lists. SSRIs like sertraline? No major food restrictions.
What You Can Do: Simple Rules for Safer Medication Use
You don’t need to be a pharmacist to avoid dangerous interactions. Just follow these five rules:
- Read the label. Look for phrases like “take on empty stomach,” “avoid dairy,” or “do not take with grapefruit.” If it’s unclear, ask your pharmacist.
- Time matters. If your pill says “take one hour before food,” wait 60 minutes. Don’t guess. Use your phone’s alarm.
- Keep your diet steady. If you’re on warfarin, eat about the same amount of greens every day. Don’t go from kale smoothies to no veggies.
- Check for grapefruit. If you’re on a statin, blood pressure pill, or anti-anxiety med, skip grapefruit, Seville oranges, pomelos, and tangelos. Even “grapefruit-free” juice can be contaminated.
- Use a medication tracker. A 2019 study in JAMA Internal Medicine showed that patients using visual schedules cut food-drug errors by 47%. Apps like MyMedSchedule (from NIH) now use AI to build custom plans based on your meals, sleep, and meds.
What’s Changing in 2026
The system is catching up. Starting in 2024, the FDA required all new prescription labels to include clear food interaction warnings with exact timing. By 2026, they expect a 20% drop in related hospital visits. Medicare Part D now requires pharmacists to counsel seniors on food-drug risks when starting high-risk meds-this affects over 12 million people annually.
Genetic testing is also entering the picture. If you regularly eat grapefruit and are prescribed a statin, your doctor might now test you for CYP3A4 enzyme activity. People with slow metabolism are 4x more likely to have dangerous drug buildup. This test isn’t routine yet-but it’s coming.
The biggest change? Awareness. In 2024, the American Pharmacists Association found that 54% of patients didn’t know grapefruit could interact with their meds. That number is dropping-thanks to clearer labels, pharmacist counseling, and better apps.
Final Thought: Your Food Is Part of Your Treatment Plan
Your medicine isn’t just a pill. It’s part of a system that includes your meals, your schedule, and your habits. A missed dose, a grapefruit, or a late dinner can undo weeks of treatment. But when you understand how food and drugs work together, you take control. You’re not just following rules-you’re protecting your body.
Don’t assume your doctor knows what you eat. Don’t assume your pharmacist will ask. Ask yourself: “When was the last time I checked if my food was safe with my meds?” That’s the first step to staying safe-and healthy.
Can I take my medication with a small snack if I have a sensitive stomach?
It depends on the medication. For most drugs that require an empty stomach-like levothyroxine, tetracycline, or certain HIV meds-even a small snack can reduce absorption by 30% or more. If your stomach is upset, talk to your doctor. They may switch you to a different drug that’s safer with food. Never assume a little food is okay unless the label or your pharmacist says so.
Is it safe to drink coffee with my pills?
Coffee can interfere with some medications. It can speed up how fast your body processes thyroid meds, antidepressants, and some asthma drugs. For others, like levothyroxine, caffeine can reduce absorption. If you drink coffee with your meds, you risk under-dosing. Wait at least 30 minutes after taking your pill before having coffee. If you’re on a medication with a narrow therapeutic window (like warfarin or lithium), it’s best to avoid coffee altogether during dosing times.
Do herbal supplements count as food in these interactions?
Yes. Supplements like St. John’s Wort, garlic, ginkgo, and vitamin E can interact with medications just like food. St. John’s Wort can cut the effectiveness of birth control, antidepressants, and heart meds by up to 60%. Garlic and ginkgo can thin your blood, making warfarin dangerously strong. Always tell your doctor and pharmacist about every supplement you take-even if you think it’s “natural.”
What if I forget to take my pill on an empty stomach? Should I retake it?
Don’t double up. If you took your pill with food, wait until the next scheduled dose. Taking extra can be dangerous. For example, if you took a statin with grapefruit juice, doubling the dose could lead to muscle breakdown and kidney damage. Call your pharmacist for advice. They’ll tell you if it’s safe to wait or if you need to adjust your schedule.
Can I use a pill organizer if I take meds at different times relative to meals?
Yes-but only if it’s designed for timing. A standard pill organizer won’t help if you need to take one pill an hour before breakfast and another two hours after lunch. Use a digital tracker like MyMedSchedule or a simple printed chart with time slots. Some pharmacies offer custom organizers with labeled time windows. If you’re unsure, ask your pharmacist to help you set one up.
Food-drug interactions aren’t complicated-but they demand attention. A small change in your routine can mean the difference between feeling better and ending up in the ER. Stay informed. Stay consistent. And never assume your medicine works the same way no matter what you eat.