Why Your Eczema Won’t Go Away
Most people think eczema is just dry, itchy skin. But if you’ve had it for years, you know it’s deeper than that. It’s not just a rash that comes and goes. Chronic eczema - usually called atopic dermatitis - is a broken skin barrier that won’t heal on its own. And until you fix that barrier, nothing else works long-term. The itch? That’s just the symptom. The real problem is your skin’s protective layer is crumbling, letting in irritants, bacteria, and allergens. Studies show this damage happens 3 to 6 months before the first flare-up in babies at risk. If you’re still using basic lotions and hoping for relief, you’re treating the fire, not the spark.
What’s Actually Broken in Your Skin
Your skin isn’t just a surface - it’s a layered fortress. The top layer, called the stratum corneum, is made of dead skin cells held together by lipids: ceramides, cholesterol, and free fatty acids. In healthy skin, these lipids form tight, brick-and-mortar walls. In chronic eczema, those walls are cracked. Ceramide levels drop by 30-50%, especially the long-chain ceramide 1 that keeps moisture locked in. Your skin’s natural pH, which should be around 5.0, rises to 6.5 or higher. That throws off enzymes that rebuild lipids, making repairs impossible. And if you have a mutation in the filaggrin gene (which 50% of moderate-to-severe cases do), your body can’t even make enough of the proteins that hold those bricks together. That’s why some people’s skin just won’t heal - their blueprint is damaged.
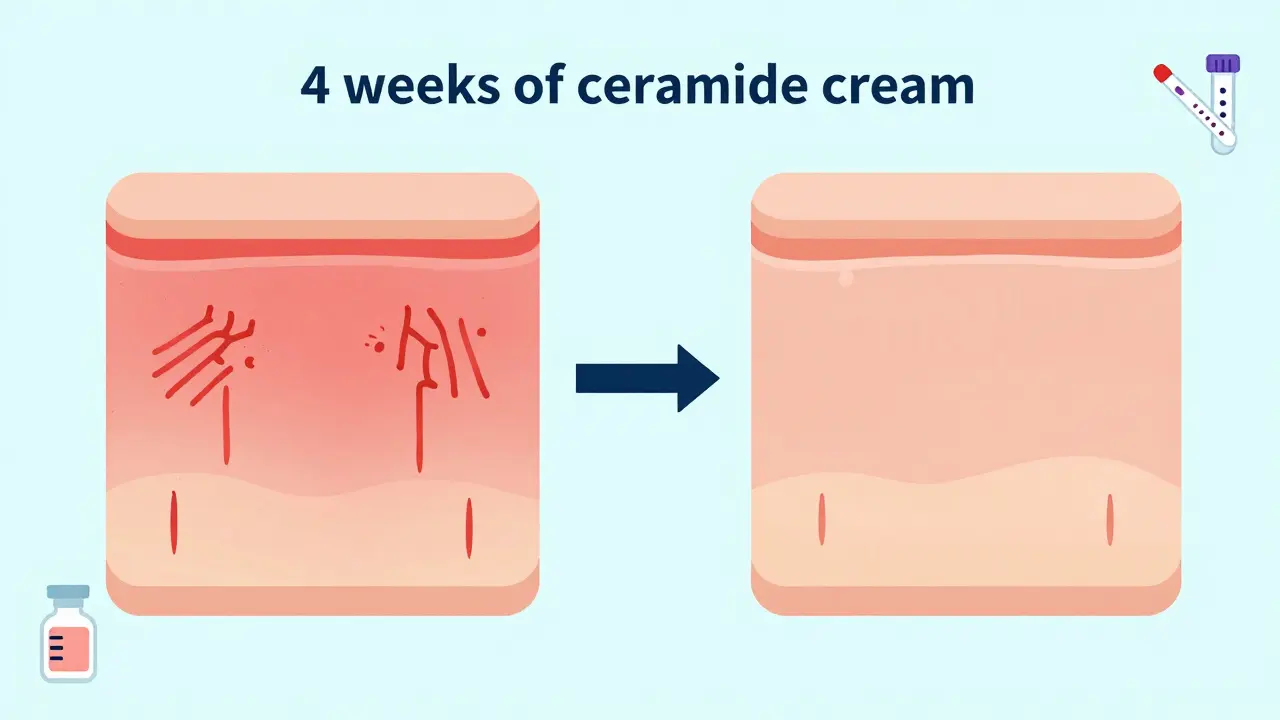
Barrier Repair Isn’t Just Moisturizing - It’s Rebuilding
Regular moisturizers? They sit on top. They give temporary relief, but they don’t fix the cracks. True barrier repair uses lipids that match your skin’s natural composition. The gold standard is a 1:1:1 ratio of ceramides, cholesterol, and free fatty acids. Products with this formula restore the skin’s lipid matrix. Clinical trials show they reduce water loss (TEWL) by 30-50% in just two weeks. That’s not a guess - it’s measured with instruments in labs. One study found these formulations were 87% effective at repairing the barrier, while basic petrolatum or glycerin creams only worked 52% of the time. You don’t need fancy ingredients. You need the right ones in the right amounts. Look for products with 3-5% ceramides, 2-4% cholesterol, and 1-3% free fatty acids. Brands like CeraVe, EpiCeram, and Atopiclare use this science. Avoid anything with alcohol, fragrance, or parabens - they make the damage worse.
Triggers Aren’t Just Allergens - They’re Stressors Your Skin Can’t Handle
You’ve heard “avoid dust mites” or “stop eating dairy.” But triggers aren’t always obvious. Sweat, hard water, harsh soaps, and even low humidity can crack your barrier further. A 2023 study showed that washing with water above 100°F (38°C) strips lipids 40% faster than lukewarm water. Fragrance in laundry detergent? That’s a trigger. Wool sweaters? They rub and irritate. Even emotional stress raises cortisol, which weakens your skin’s defense. The biggest trigger most people miss? Over-washing. Showering twice a day, scrubbing with loofahs, using antibacterial soaps - all of this destroys what little barrier you have left. You don’t need to eliminate every trigger. You need to reduce them. Use a humidifier in winter. Wear cotton. Switch to fragrance-free detergent. Rinse off sweat within 15 minutes. Small changes add up.

How to Stop the Itch Without Steroids
Itch is the worst part. It keeps you up at night. It leads to scratching, which breaks the skin, which causes infection, which makes it itch more. It’s a loop. Topical steroids help fast - they reduce inflammation in days. But they thin your skin over time. A 2022 study showed 15-20% reduction in stratum corneum thickness after just 6 weeks of daily use. That’s not a fix - it’s a trade-off. Instead, focus on breaking the itch-scratch cycle at its source: the barrier. When your barrier is repaired, itch drops by 60-70%. Why? Because the nerve endings in your skin aren’t being bombarded by irritants anymore. For immediate relief, use cool compresses, pat instead of scratch, and try menthol or pramoxine creams (available OTC). For stubborn cases, pimecrolimus cream (1%) works without thinning the skin. It doesn’t work as fast as steroids, but it builds your skin back up while calming inflammation. One patient on Reddit tracked her itch for 30 days after switching to a ceramide cream: “Nighttime scratching dropped from 5 times to once. I slept through the night for the first time in 3 years.”
How to Apply Barrier Creams Right (Most People Get It Wrong)
Applying cream once a day? That’s not enough. The American Academy of Dermatology says you need twice daily - morning and night. And you have to do it right. After a bath or shower, pat your skin dry - don’t rub. Then apply within 3 minutes. That’s when your skin is still holding water. Use about 5 grams per arm (that’s two fingertip units). For your torso and legs, use 10-15 grams total. Don’t skip the elbows, knees, and neck - those are hotspots. Wait 15 minutes before applying any steroid or anti-itch cream. If you put them on together, the barrier cream blocks absorption. And yes, it will feel greasy at first. That’s normal. Most people quit because of the texture. But 85% of users adapt within two weeks. Watch instructional videos from EpiCeram or MyEczemaTeam. Seeing the right technique makes a huge difference.
When Barrier Repair Alone Isn’t Enough
Here’s the hard truth: barrier repair works for 60-70% of people. But if you have a severe filaggrin mutation, your skin might not respond - even with perfect use. Studies show TEWL stays above 45 g/m²/h in these cases, meaning your skin leaks moisture too fast for creams to fix. If you’ve been using a high-quality ceramide cream for 12 weeks with no change, talk to your doctor. New options like JAK inhibitors (abrocitinib, upadacitinib) target the immune system at the root. They’re pills or injections, not creams. They don’t fix the barrier, but they calm the inflammation so your skin can heal. One 2023 case study showed a 7-year-old reduced steroid use by 80% after starting a JAK inhibitor + barrier therapy combo. This isn’t failure. It’s progression. Your body might need a two-pronged approach.
Cost, Insurance, and What’s Coming Next
Good barrier creams cost $25-$30 for 200g. Basic lotions? $10. That’s a big difference. Medicare covers prescription barrier products like EpiCeram - but not over-the-counter brands. Private insurance varies. If cost is a barrier, look for generics. Some pharmacies offer ceramide blends at half the price. And don’t forget: if you’re spending $50 a month on steroids, antihistamines, and wipes, you’re already spending more than a good barrier cream. Long-term, repair saves money. The future is personalization. Companies like Dermavant are partnering with 23andMe to match your filaggrin mutation with the right lipid formula. By 2026, you might get a skin test and a custom cream in the mail. Emerging therapies like platelet-rich plasma (PRP) are being tested to boost filaggrin production by 300%. Sustainability is also becoming a factor - the EU now requires 30% biodegradable ingredients in barrier creams by 2027. The old silicones? They’re being phased out.
What Works - Real Results From Real People
On Reddit’s r/Eczema, 78% of 1,200 users reported major improvement with ceramide-based creams. One user wrote: “TEWL went from 38 to 15 after 30 days. I stopped using steroids.” On Amazon, ceramide creams average 4.2 out of 5 stars from over 12,500 reviews. The top comments: “No more 3 a.m. scratching,” “Flares dropped from weekly to monthly,” “My skin finally feels like skin again.” But 35% said the first few applications stung - especially on open cracks. That’s not an allergy. It’s your skin reacting to the pH. Wait a few days. It fades. And 62% on MyEczemaTeam say the cost is unsustainable. That’s why consistency matters more than brand. Use what works, even if it’s a generic. The science doesn’t care what’s on the label - it cares about the lipid ratio.
Bottom Line: Fix the Barrier, Then Everything Else Follows
Chronic eczema isn’t a mystery. It’s a broken skin barrier. You can’t out-itch it. You can’t out-steroid it. You can’t out-moisturize it. You have to rebuild it. Start with a ceramide-cholesterol-free fatty acid cream, applied twice daily after bathing. Avoid triggers you can control. Give it 4 weeks. If you see less itching, fewer flares, and better sleep - you’re on the right path. If not, talk to a dermatologist about JAK inhibitors or genetic testing. This isn’t about quick fixes. It’s about long-term skin health. And if you’ve been struggling for years, this might be the first real solution you’ve tried.

12 Comments
Write a comment