If you live with low phosphate, the thing that wrecks a trip isn’t the long flight or the noisy hotel. It’s small, fixable stuff-missed doses, a sprint through a terminal without a snack, a bout of diarrhea-stacking up until your legs feel like concrete and your brain lags a second behind your body. You can’t control everything on the road, but you can control enough. This guide keeps it real: what to pack, how to dose across time zones, what to eat when choices are grim, and when to get help. I’m Benjamin, based in Wellington with two kids (Ansel and Neri) who’ve turned layovers into Olympic sports. These are the habits that keep me-and readers I help-moving.
TL;DR: Low-Phosphate Travel, Made Manageable
- Carry 1.5× your meds in your carry-on, with a doctor’s letter and original labels. Split backups across bags. Keep doses tied to meals and set phone alarms.
- Time zones: keep the usual spacing between doses. Shift your schedule 1-2 hours per day until you match local time. Don’t double up after a miss; restart at the next dose.
- Food: anchor every meal with protein (eggs, yogurt, meat, tofu, beans). Time calcium/iron/antacids 2 hours away from phosphate. Pack ORS (oral rehydration) for diarrhea.
- Flights, altitude, heat, or heavy drinking can push phosphate down. Breathe slow, hydrate, avoid big fasts followed by huge meals, and go easy on alcohol.
- Red flags (urgent care): severe weakness, chest pain, confusion, trouble breathing, dark urine, or a racing/irregular heartbeat. For kids with XLH, get help early if they stop eating or can’t keep meds down.
Sources I trust when building this: UpToDate clinical reviews (2024-2025), NICE NG7 on refeeding syndrome (latest update), ASPEN consensus (2020) on refeeding risk, international XLH guidance (2022), and government travel-medicine carriage rules like Medsafe NZ and airport security guidance for medically necessary liquids.
Before You Go: Plan Like a Pro
Start 2-4 weeks before departure. Quick prep now saves the messy stuff later.
- Know your pattern. Are you managing chronic low phosphate (like XLH or tubulopathies), or are you prone to dips during illness, fasting, hard training, or heavy alcohol? Your plan follows your pattern.
- Check in with your clinician. Ask if you need labs pre‑trip (phosphate, calcium, creatinine, ALP, PTH, vitamin D). Confirm your dose plan and a “sick‑day” plan (what to do with vomiting, diarrhea, or missed doses). If you’re on calcitriol/alfacalcidol or burosumab, confirm timing and monitoring.
- Write down targets and symptoms. Know your usual phosphate range and the symptoms that mean you’re drifting (for many: new muscle weakness, bone pain, brain fog, tingling, shortness of breath on stairs).
Medication and documents checklist:
- Bring 1.5× your planned number of doses. Keep the full set in your carry‑on in original labeled containers. Split a small reserve into another bag.
- Carry a doctor’s letter listing diagnoses, meds (generic names and doses), devices (e.g., syringes/gel packs for injectables), and medically necessary liquids. Security agencies allow these when declared.
- Have paper prescriptions and digital copies. Ask for a script using generic names (e.g., sodium/potassium phosphate, calcitriol). Brand names vary by country.
- If on burosumab: confirm your injection window, cold‑chain plan, and disposal for sharps. The manufacturer’s patient support can help coordinate abroad; loop them in early.
- Pack ORS packets and a small pill organizer labeled by time of day. Include a thermometer and a simple symptom log (paper or phone note).
Insurance and access:
- Declare pre‑existing conditions when buying travel insurance so emergencies and med replacements are covered. Confirm outpatient labs and medicines are included.
- Ask your clinician for a lab request you can reuse if symptoms hit. Many labs accept emailed referrals; telehealth follow‑ups help you course‑correct.
- Check medicine import rules where you’re going. Many countries allow up to 3 months’ personal supply with a prescription and original labels (Medsafe NZ gives that guidance locally; other countries have similar rules but always check).
Special groups:
- Pregnancy: discuss plans early-phosphate, calcium, and vitamin D balance changes.
- Kids with XLH: confirm dosing intervals, appetite strategies on travel days, and who to call if vomiting or diarrhea starts.
- Diabetes or malnutrition risk: you’re at higher risk for refeeding‑related drops; carry ORS and small frequent snacks; review the plan for meals after long fasts.
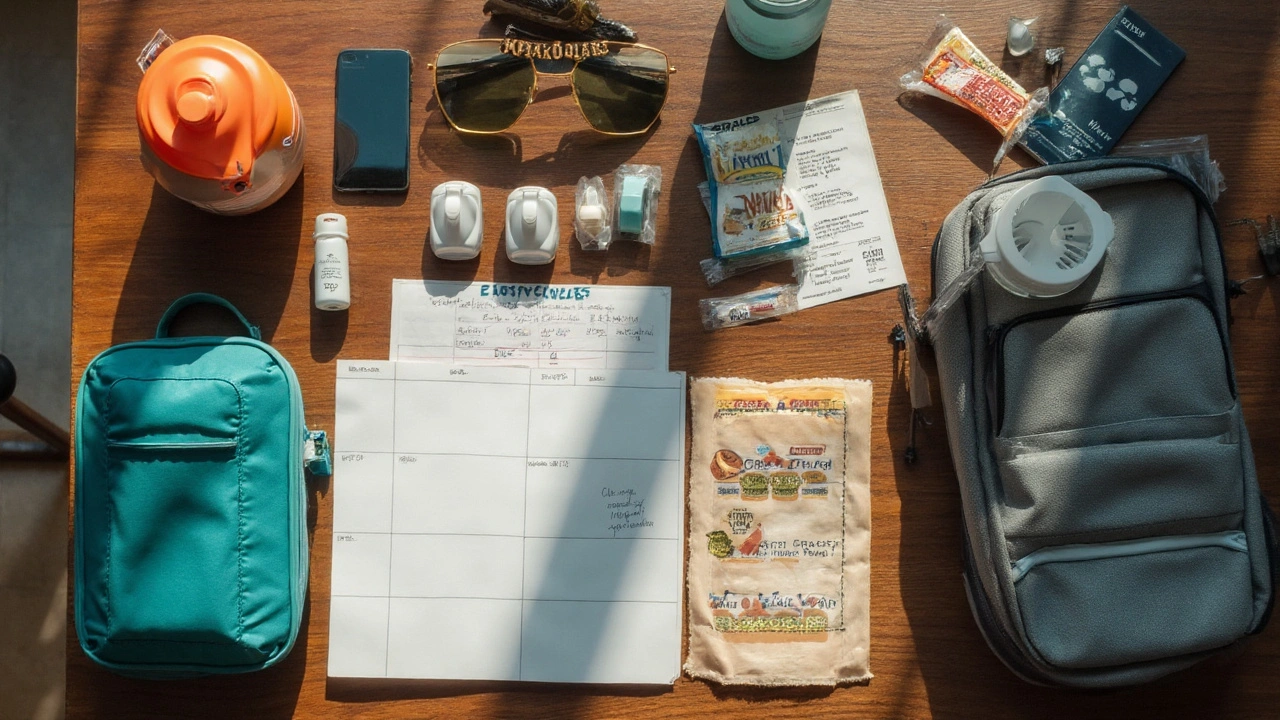
Personal tip: I keep our kits simple. Each person gets a zip pouch: meds, ORS, a letter, and a snack that counts (Greek yogurt or cheese and crackers). My kids know the drill-snack before we sprint.
Meds and Time Zones: Stick the Landing
Meds keep you steady. Travel tries to break the rhythm. Here’s how to keep it together without math headaches.
Dosing basics (always follow your clinician’s specifics):
- Phosphate salts (sodium or potassium phosphate) usually work best in small, divided doses with food to reduce stomach upset. If you miss a dose and it’s within ~3 hours, take it; otherwise skip and take the next dose on time. Don’t double up.
- Vitamin D analogs (calcitriol/alfacalcidol) are once or twice daily. Keep them on schedule because they affect phosphate handling and calcium.
- Burosumab (for XLH) is given every 2-4 weeks. If your injection falls during the trip, schedule it just before you leave, or plan a cold‑chain day with a clinic abroad.
- Avoid binders at the wrong time: calcium, iron, aluminum/magnesium antacids, sucralfate, and cholestyramine can block phosphate absorption. Keep them 2 hours away from your phosphate dose.
- Other meds that can lower phosphate: insulin/dextrose infusions, high‑dose beta‑agonists (e.g., frequent salbutamol), theophylline, some diuretics. Use what you need, but be aware and keep nutrition steady.
Time‑zone rule of thumb (no spreadsheets required):
- Protect the spacing between doses. If you usually dose with breakfast/lunch/dinner, keep doing that at local meal times.
- Shift gently: move your dosing 1-2 hours per day toward the new time zone until you’re synced. Long‑haul to Europe from NZ? Take your next dose at the next local meal; the spacing fixes itself over 1-2 days.
- Red‑eye flights: set alarms for key doses; if you’re asleep and it’s a middle‑of‑the‑night dose, skip it and resume at breakfast unless your clinician told you otherwise.
Flight day specifics:
- Keep meds in your personal item under the seat (not the overhead) so you can get to them when the seatbelt sign stays on.
- Pair doses with a real snack. A yogurt cup or milk at the airport beats a dry biscuit and helps absorption.
- Stomach sensitive? Take smaller, more frequent doses those first 24 hours instead of one big hit.
Storage and backups:
- Most tablets and capsules are fine at room temp; avoid heat and car gloveboxes. If you need cooling, use gel packs and a small insulated pouch.
- List the generic names on your phone. If your bag goes missing, a pharmacist abroad can match the ingredients even if the brand is different.
- Set two reminders for each dose (one at time, one 15 minutes later). On busy travel days you’ll thank your past self.

Eat, Drink, Move: Day-to-Day Controls
Food and fluids are your quiet stabilizers. You don’t need perfect choices-just steady ones.
Build each meal around protein:
- Breakfast ideas on the road: eggs, Greek yogurt, cottage cheese, tofu scramble, smoked fish, bean‑and‑cheese wrap.
- Lunch/dinner: chicken, beef, lamb, fish/shellfish, beans and rice, lentil dal, tofu/tempeh, peanut butter sandwich when options are bleak.
- Snacks: milk, kefir, cheese and crackers, trail mix with nuts/seeds, hummus with pita, protein shakes you tolerate.
Timing tips:
- Take phosphate with or right after food to ease GI upset.
- Space calcium or iron supplements 2 hours away from phosphate doses.
- If you also have kidney disease, do not push high‑phosphate foods without a clear plan from your nephrologist.
Hydration that actually helps:
- Carry a bottle. Aim for pale‑yellow urine. On flights, drink a cup of water every hour you’re awake.
- At the first hint of diarrhea, switch to ORS (oral rehydration solution). It’s better than water alone for keeping electrolytes balanced.
- Easy ORS rule: one standard packet in 200-250 mL water, sip steadily. If you run out, use sports drinks lightly diluted plus salty crackers until you restock.
Alcohol, caffeine, and soda:
- Alcohol can drive poor intake and worsen dips. Set a limit before you start. Alternate with water, eat before you drink, and skip the nightcap on hard travel days.
- Caffeine is fine in moderation, but it’s not hydration. Match each coffee with water.
- Cola has phosphate, yes, but it’s not a treatment. If you need an emergency snack pairing for a dose, choose milk/yogurt or a protein‑rich option over soda.
Stomach bugs and food safety:
- Eat foods that are cooked and hot. Peel fruits yourself. Skip buffet sushi at midnight.
- For non‑bloody travelers’ diarrhea, loperamide can be helpful, but if you also have fever or blood, seek care. Keep taking ORS.
- If vomiting prevents meds for more than 12-24 hours (or sooner in kids), get help.
Movement without a crash:
- Warm up longer than usual; avoid all‑out efforts after long flights.
- If you’re hiking at altitude, add a snack every 60-90 minutes and pace your breathing.
- Heavy strength sessions on day one? Save them for when sleep debt clears.
Flights, Altitude, Heat, and Illness: Avoid the Common Traps
Certain settings nudge phosphate lower. Knowing the why helps you dodge the worst.
Flights and altitude:
- Breathing fast (anxiety, thin air) lowers CO₂, which shifts phosphate into cells, dropping blood levels. On planes or at altitude, slow your breathing: in for 4, out for 6, through the nose if you can.
- Plan for an extra snack during long climbs or after airport sprints. Small, frequent calories beat a feast after a fast.
- Altitude meds like acetazolamide can change your acid‑base balance and increase urination; talk to your clinician about whether it’s right for you and how it plays with your phosphate plan.
Heat and sweat:
- Heat pushes fluids out and kills appetite. Set a water timer on your watch. Pair water with salty snacks or ORS during long, hot days.
- Don’t count iced coffee as hydration. It’s fine, just not your base.
Illness and refeeding risk:
- If you’ve had poor intake for a few days, a big carb‑heavy meal can drop phosphate fast (classic refeeding pattern). Start with smaller mixed meals and step up over 24-48 hours. This follows guidance from NICE NG7 and ASPEN’s consensus.
- Alcohol binges, sepsis, diabetic episodes, and certain meds can all tilt phosphate downward. Keep doses steady and call your clinician sooner rather than later.
When to seek urgent care:
- Severe, new muscle weakness or you can’t climb one flight of stairs you could do last week.
- Chest pain, severe shortness of breath, fainting, new palpitations, or confusion.
- Dark/brown urine, severe cramps, or severe vomiting/diarrhea with signs of dehydration.
- For kids: reduced eating/drinking with lethargy, or vomiting that blocks meds-get help early.
What I do in real life: I keep a one‑page card in my wallet-diagnosis, meds, usual dose times, allergies, and an emergency contact. If something goes sideways in a strange city, I’m not relying on my tired brain to remember details.
Quick Tools: Checklists, Decision Tree, FAQ
Bookmark this section. These are the pieces you’ll actually use at the gate, in a hostel kitchen, or at 3 a.m. after a missed connection.
Carry‑on packing list:
- Meds: 1.5× supply, original containers, pill organizer, paper prescriptions.
- Doctor’s letter for security and customs.
- ORS packets, small snacks (protein first), collapsible bottle.
- Thermometer, hand sanitizer, basic first aid (loperamide, paracetamol, any regular meds).
- Phone note with your diagnoses, meds (generic names), doses, and emergency contacts.
Time‑zone dosing cheat sheet:
- Day 0 (travel): take doses with meals you actually eat.
- Day 1-2: shift dose times toward local meals by 1-2 hours per day.
- Always keep a 2‑hour gap from calcium/iron/antacids.
- Missed dose? If you remember within ~3 hours, take it. If not, skip and go on schedule.
Food shortlist for airports and stations:
- Milk or kefir, Greek yogurt cups, cheese and crackers.
- Egg sandwich, tuna wrap, chicken salad, tofu bowl.
- Nuts/seeds trail mix, hummus with pita, protein bars you tolerate.
Decision tree: “I feel off-what now?”
- Mild (tired, light weakness, mild brain fog):
- Eat a protein‑rich snack and take your next scheduled dose.
- Drink 300-500 mL water; add ORS if you’ve had diarrhea or lots of sweat.
- Slow breathing for 5 minutes if you’re anxious or at altitude.
- Reassess in 1-2 hours.
- Moderate (stairs feel hard, cramps, new tingling, poor appetite):
- Hydrate with ORS, eat a proper meal within 30-60 minutes, and rest.
- Check meds for timing conflicts (calcium/iron/antacids too close?). Fix spacing.
- If not improving by the next dose window, call your clinician or local urgent care.
- Severe (can’t stand without help, chest pain, confusion, dark urine, new fast/irregular heartbeat):
- Seek emergency care now. Show your med list and condition card.
Mini‑FAQ
- Can I fly with this condition? Yes, most people can. Keep doses steady, hydrate, eat regularly, and manage breathing if you’re anxious. If you’ve had recent severe hypophosphatemia, ask your clinician before long‑haul or high altitude.
- Do I need airport approval for my meds? Medically necessary liquids, gel packs, and syringes are allowed when declared and screened. Bring your letter and original labels.
- What if I vomit after a dose? If it’s within 15 minutes, assume the dose didn’t stay down; once your stomach settles, take a light snack and try again. If vomiting continues or you can’t keep meds down for 12-24 hours (earlier for kids), get help.
- Can I use cola to “fix” low phosphate? Don’t. It’s not reliable and it’s rough on health. Choose dairy, yogurt, or a protein meal with your dose.
- How do I handle multi‑day hikes? Pre‑portion doses by day, add a snack every 60-90 minutes, sip ORS during long climbs, and plan earlier bedtimes. If you’re going very high, discuss a plan first.
- XLH on burosumab: travel timing? Many schedule an injection just before travel. If you must inject abroad, arrange a clinic visit and cold chain ahead of time and carry documentation for security.
Next steps and troubleshooting by scenario
- Weekend city break, 2-3 hours time change: Keep doses with meals, don’t overthink the clock. Pack two ORS packets and a protein snack for each travel day.
- Long‑haul (10-12 hours) with kids: Pre‑load snacks in your bag. Set shared phone alarms for dose times. I hand my kids a yogurt before we board and another after takeoff-zero negotiations later.
- Work trip with nonstop meetings: Block 10 minutes on your calendar for snack + dose. People respect calendar blocks more than “I’ll find a minute.”
- Adventure travel (heat/altitude): Plan a snack every hour you’re exerting. Carry two ORS packets/day in your pack. Pace breathing on climbs.
- History of refeeding dips: After any long fast (jet‑lagged day, illness), start with a small mixed meal, then step up. Keep phosphate doses small and regular. If you feel woozy or weak, don’t “feast”-split meals.
What backs this up (plain‑English citations):
- UpToDate’s hypophosphatemia reviews (2024-2025) on causes, symptoms, and treatment emphasize divided dosing and watching for triggers like alkalosis, insulin, and illness.
- NICE NG7 and the 2020 ASPEN consensus outline refeeding risk and support slow, structured re‑nutrition with electrolyte monitoring.
- International XLH guidance (2022) covers treatment timing, vitamin D analogs, and burosumab logistics important for travel.
- Security and customs bodies (e.g., Medsafe NZ for personal meds import; airport security policies for medical liquids) allow reasonable amounts when documented and declared.
Last word from the road: your best friend is a routine you can keep on a bad day. For me that’s simple-dose with food, small steady snacks, water in hand, and alarms doing the remembering. It’s not glamorous. It works.
Use these hypophosphatemia travel tips as your core playbook, then tweak with your clinician’s advice to fit your specific condition and meds.
Just got back from a 14-hour flight with my kid who has XLH and this guide was a lifesaver. We packed yogurt cups, set dual alarms, and didn’t even think about soda once. The snack-before-sprint rule? Genius. I cried a little when we landed and she didn’t look like a zombie.
i was just wondering if anyone else uses a pill organizer with time labels? i keep misplacing mine and end up taking doses at weird times… also, does anyone know if ors packets expire? mine are from 2022 and i’m scared to use them 😅
Y’all need to stop treating this like a travel blog and start treating it like a survival manual. This isn’t ‘snack before sprint’-this is your body screaming for phosphate and you’re out here with a granola bar. I’ve seen people crash on planes because they thought ‘protein’ meant ‘peanut butter packet.’ Wake up. You’re not camping. You’re managing a chronic metabolic condition.
I’m so grateful for this post. As someone with XLH and a history of refeeding syndrome, I’ve spent years learning the hard way that ‘just eat more’ is dangerous advice. The decision tree here? Perfect. I printed it, laminated it, and keep it in my wallet next to my emergency card. Also-slow breathing on flights? I didn’t know that was a thing. Turns out, I was hyperventilating every time the seatbelt sign lit up. Now I do 4-6 breathing. It’s like a mini meditation. Thank you, Benjamin.
While the practical advice is sound, I must note that the reliance on anecdotal evidence from personal experience, however well-intentioned, risks diluting the clinical rigor of the recommendations. The referenced guidelines are appropriate, but the framing occasionally blurs the line between medical protocol and lifestyle hack. Precision matters in electrolyte management.
As someone from India managing hypophosphatemia while traveling across South Asia, I can tell you-this guide is gold. The ORS advice? Spot on. In Delhi, I once used a local ‘chaas’ (spiced buttermilk) with a pinch of salt and sugar as a makeshift rehydration solution. Works better than some commercial stuff. Also, in rural areas, boiled eggs and lentils are your best friends. Protein is everywhere if you know where to look. And yes, the ‘2-hour gap’ rule? Non-negotiable. I’ve seen people take calcium supplements with breakfast and then phosphate at lunch-total waste. Your body doesn’t care about your schedule.
Let’s be honest-this guide assumes you have access to refrigeration, clean water, and pharmacies with generic sodium phosphate. What about travelers in low-resource settings? The ‘Greek yogurt’ suggestion is great if you’re in Zurich. In rural Nepal, it’s a boiled egg and a banana. The ‘1.5x meds’ rule is ideal, but what if your meds get confiscated? Or if you’re flying through a country that doesn’t recognize your diagnosis? This reads like a first-world checklist. Real-world management is messier.
Wow. So we're now treating phosphate as if it's a magic bullet? You're telling people to 'anchor meals with protein' like it's a TikTok trend. And burosumab? You're asking people to coordinate cold-chain logistics abroad like it's a Netflix documentary. This isn't travel advice. It's corporate wellness propaganda dressed up as patient empowerment. Next you'll be selling branded protein bars with QR codes to your doctor's email.
Thank you for the comprehensive and clinically grounded guidance. The integration of UpToDate, NICE NG7, and ASPEN standards demonstrates a commendable commitment to evidence-based practice. I particularly appreciate the emphasis on dose spacing, avoidance of concomitant calcium/iron administration, and the structured approach to time-zone adaptation. As a healthcare provider, I will be distributing this resource to my patients with hypophosphatemic conditions. The inclusion of pediatric considerations and refeeding risk mitigation is especially valuable.
Man, I wish I had this when I flew to Tokyo last year and ended up in the ER after missing two doses because I thought ‘I’ll just eat more rice.’ Didn’t know phosphate wasn’t in rice. Didn’t know cola wasn’t a fix. Didn’t know slow breathing mattered. I spent three days in a hospital bed wondering why my legs felt like wet noodles. This guide is the kind of thing you wish existed before you become a statistic. Thank you for writing it. I’m printing 3 copies.
Okay but can we talk about how OBSESSED Benjamin is with yogurt? Like, is this a sponsored post? 🤔 I’ve been doing this for 12 years and I’ve never once used yogurt. I use protein powder in water. And why is everyone acting like this is the first time anyone’s ever talked about phosphate? This is basic nephrology 101. Also-why are we letting a guy from Wellington write global guidelines? What about people in the Global South? Do they just… not exist? 🤷♀️
I’ve been living with XLH since I was 4, and I’ve traveled to over 30 countries. I can tell you-this guide nails the emotional weight of it. It’s not just about the meds. It’s about the fear. The panic when you’re in a foreign airport and your stomach is churning and you can’t find a yogurt. The guilt when your kid’s legs shake because you forgot the snacks. The way you start calculating time zones like a mathematician just to get your dose right. This isn’t a checklist. It’s a lifeline. And the part about ‘your best friend is a routine you can keep on a bad day’? That’s the truth no one else says out loud. Thank you.
EVERYTHING IS A CONSPIRACY. The WHO, big pharma, and airport security are all in cahoots to make you think phosphate is a ‘problem.’ They don’t want you to know that low phosphate is just your body’s way of detoxing from modern processed foods. The ‘dose with food’ thing? That’s a placebo. The real fix is alkaline water, sunlight, and avoiding fluoride. And those ‘gel packs’? They’re tracking your location. The ‘doctor’s letter’? That’s your signature on the surveillance contract. Wake up. You’re being gaslit into dependency.
Hey I just wanted to say this is amazing and I’m sharing it with my whole family. My mom has low phosphate and she’s been avoiding travel for 10 years because she’s scared. Now she’s booked a trip to Florida. Also, can I ask-do you have a printable version of the decision tree? My phone died in the airport last time and I couldn’t find it. Thanks so much!! 😊
OMG I LOVE THIS SO MUCH 🥹 I printed it out and stuck it in my travel journal next to my passport 📄✨ The yogurt tip? Changed my life. Also, I made a little Pinterest board called ‘Hypophosphatemia Travel Vibes’ with pics of my protein snacks and pill organizers 🥛🥚 #PhosphateQueen #TravelWithPurpose
Let me get this straight-you’re telling Americans to carry ‘ORS packets’ like we’re in some third-world country? We have Gatorade. We have Powerade. We have protein shakes in every gas station. This isn’t survival. This is fear-mongering. And why are we letting a Kiwi tell us how to manage our health? This isn’t a global pandemic, it’s a personal condition. We don’t need your ‘cold-chain’ nonsense. We’ve got refrigerators. We’ve got pharmacies. We’ve got common sense.
Thank you for writing this. I’m a nurse in rural Maine and I’ve had patients cancel trips because they didn’t know how to manage their meds. This guide is clear, compassionate, and practical. I especially love the ‘mild/moderate/severe’ decision tree-it’s something I’ve been trying to create for years. I’ve already shared it with my clinic’s travel health team. One small thing: typo in ‘orthography: typo-prone’-you wrote ‘Orthography’ with a capital O in the traits list. Just saying. 😊
While the intent of this guide is laudable, the presentation lacks scholarly rigor. The conflation of clinical recommendations with anecdotal personal experience undermines its authority. Furthermore, the absence of peer-reviewed citations for the ‘breathing technique’ and ‘snack before sprint’ assertions renders these as heuristic suggestions rather than evidence-based interventions. A more formal structure, with references indexed to specific guidelines, would enhance its credibility in a medical context.