When your back flares up, your knees ache from arthritis, or labor contractions hit hard, reaching for a pill isn’t always the best or safest option. That’s where TENS therapy comes in - a simple, drug-free tool that uses mild electrical pulses to quiet pain signals before they reach your brain. Unlike opioids or even NSAIDs, TENS doesn’t change your chemistry. It doesn’t make you drowsy or wreck your stomach. It just interrupts the pain. And for millions of people, that’s enough.
How TENS Therapy Actually Stops Pain
TENS stands for Transcutaneous Electrical Nerve Stimulation. That’s a mouthful, but it’s just a fancy way of saying: “electrical pulses through your skin to your nerves.” The idea isn’t new. Back in 1965, scientists Ronald Melzack and Patrick Wall proposed the Gate Control Theory - the idea that your spinal cord has a kind of gate that can block pain signals if you turn up other sensations, like touch or vibration. TENS uses tiny electrical pulses to activate those non-pain signals, slamming the gate shut.
But there’s more to it. At low frequencies (2-5 pulses per second), TENS triggers your body to release its own painkillers - endorphins and enkephalins. These are the same natural chemicals your brain makes during exercise or after a good laugh. They bind to opioid receptors in your brain and spinal cord, lowering pain over time. This is why some people feel relief that lasts hours after turning the device off.
At high frequencies (50-100 pulses per second), TENS works faster but shorter. It doesn’t rely on endorphins. Instead, it floods your nerves with electrical signals so your brain gets confused. It can’t process the pain signals anymore. It’s like trying to listen to someone whisper while a loud fan is running right next to you.
What TENS Is Good For - and What It Isn’t
TENS isn’t a magic cure. But it’s proven helpful in specific situations.
- Post-surgery pain: Studies show TENS can cut opioid use by nearly 30% after procedures like knee replacements or C-sections.
- Labor pain: A 2020 Cochrane Review found women using TENS during childbirth reported 31% more pain relief than those using a placebo device.
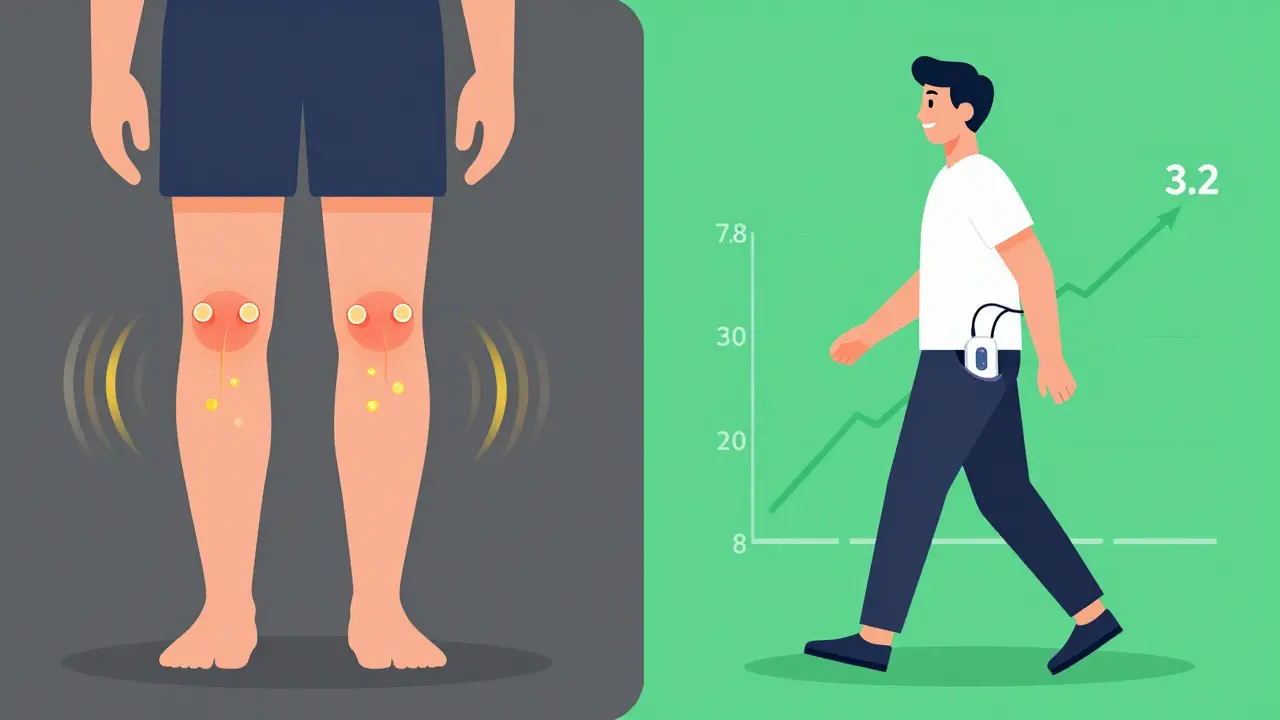
- Osteoarthritis: People with knee or hand arthritis often see a 35% drop in pain during use, compared to just 12% with fake devices.
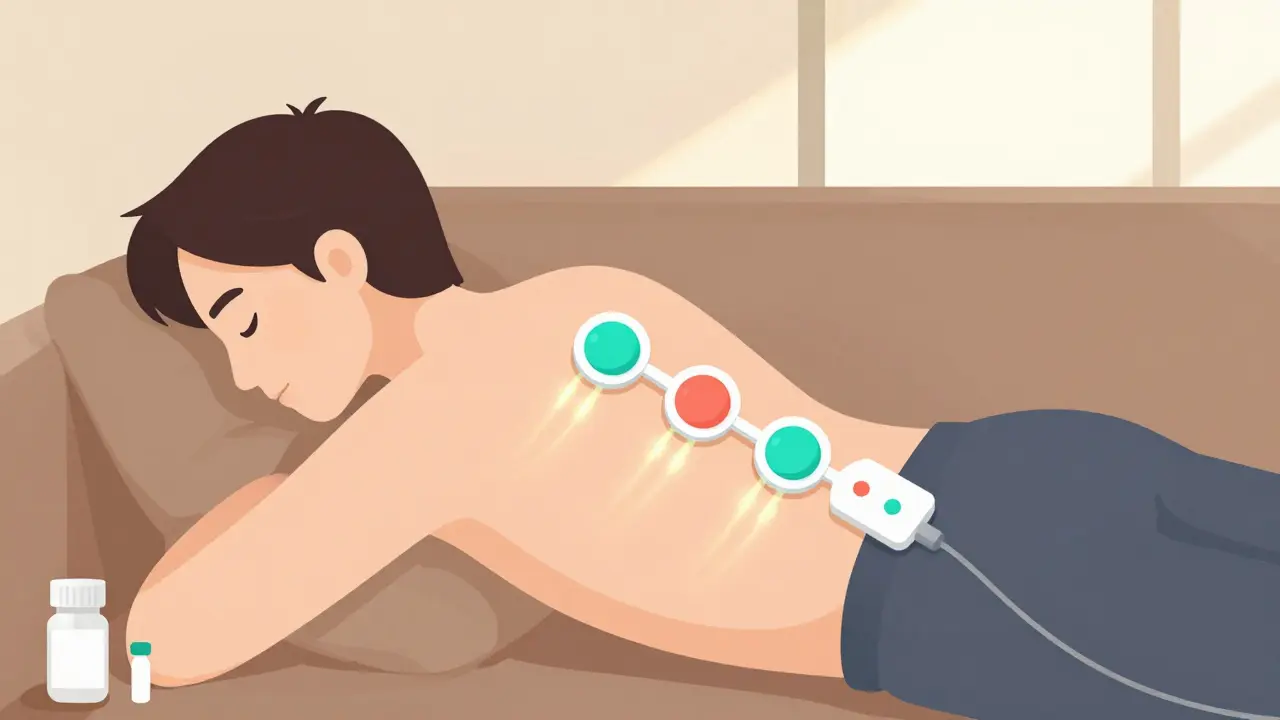
- Chronic back pain: Some users get relief, especially when electrodes are placed correctly over the spine or nerve roots. But it’s not always better than physical therapy.
Where TENS struggles? With widespread, diffuse pain like fibromyalgia. Only about 38% of those patients report meaningful improvement. It also doesn’t help much with nerve pain from diabetes or shingles unless used with precise electrode placement.
And here’s the catch: if you’re already on opioid meds, low-frequency TENS might not work as well. Your body’s opioid receptors are already occupied, so the natural painkillers TENS triggers can’t bind as easily.
How to Use a TENS Machine Right
Most people buy TENS units online or get them from a physical therapist. But buying the device is only half the battle. Getting it to work? That’s the real challenge.
Here’s what actually matters:
- Place electrodes close to the pain. Put them within 1-2 inches of where it hurts. For lower back pain, place one on each side of your spine, just above the hips. For knee pain, one above and one below the kneecap. Wrong placement? That’s why 41% of people say it didn’t work.
- Turn it up - but not too high. You should feel a strong tingling or buzzing, not pain. If it feels like a tickle, you’re not getting enough. Most failures happen because people use settings too low. A 2009 study found 68% of failed treatments used intensity below the therapeutic level.
- Choose the right mode. For sharp, recent pain (like after a sprain), use high frequency (80-100 Hz). For dull, aching pain (like arthritis), use low frequency (2-5 Hz). Some machines have “burst” mode - pulses in quick bursts - which combines both effects.
- Use it for 20-30 minutes at a time. You can use it multiple times a day, but don’t leave it on for hours. Your skin needs to breathe. And most batteries die after 8-10 hours of continuous use at full power.
Pro tip: Use conductive gel under the electrodes. Dry skin creates resistance. Gel cuts signal loss by 63%, meaning you get better pain relief with less battery drain.

Real People, Real Results
On Amazon, over 1,200 reviews show 78% of users praise TENS for immediate relief. One man with sciatica said: “It doesn’t fix my herniated disc, but it lets me walk to the mailbox without screaming.” Another woman with rheumatoid arthritis in her hands said: “I used to need ibuprofen three times a day. Now I use TENS and only take it once a week.”
But it’s not perfect. On Reddit’s r/ChronicPain, users complain about electrodes falling off during movement, skin irritation from adhesive, and machines that die after 90 minutes on high settings. One user wrote: “I crank it to 85% and it works - but the battery dies before I finish my work shift.”
A Cleveland Clinic case study followed a 54-year-old woman with chronic back pain. Her pain score dropped from 7.8 out of 10 to 3.2 in just 20 minutes of TENS use. She cut her oxycodone dose by 60% within two weeks.
What to Look for in a TENS Device
The market is crowded. You’ve got professional-grade units from Omron and Chattanooga, and cheap ones from TechCare or Amazon Basics.
Here’s what to prioritize:
- Adjustable intensity: Must go up to at least 60 mA. Lower than that won’t cut it for most pain.
- Multiple modes: High frequency, low frequency, and burst mode. Avoid single-mode units.
- Dual channels: Lets you treat two areas at once - like both knees or both sides of your back.
- Clear instructions: Some units come with 8-page manuals. Others (like Omron Max Power) have 147 pages. You need the latter.
- Rechargeable battery: Avoid units that use AA batteries if you plan to use it daily. Rechargeable lasts longer and costs less over time.
Professional clinics use TENS in 28% of cases as a first-line treatment. But they also train patients. If you’re buying on your own, consider a session with a physical therapist. Five 30-minute visits to learn placement and settings can double your success rate.
The Future of TENS: Smarter, Not Just Stronger
TENS isn’t standing still. In May 2023, the FDA cleared the first AI-powered TENS device - NeuroLoop AI. It uses sensors to read your nerve response in real time and adjusts the pulse automatically. In trials, it delivered 44% more pain relief than standard units.
Researchers at the NIH are now developing “smart electrodes” with built-in sensors that detect skin moisture and impedance. If your skin gets dry during use, the device automatically boosts power to keep the signal strong.
And big companies are taking notice. Amazon installed TENS units in 147 warehouses to help workers with back strain. They reported a 19% drop in missed workdays.
The CDC’s 2023 opioid guidelines now explicitly recommend TENS as a first-line option for chronic pain. They predict a 35% increase in prescriptions from primary care doctors by 2025.
When TENS Won’t Work - And What to Do Instead
Not everyone benefits. If you’ve tried TENS and it did nothing, don’t give up on non-drug pain relief. Here’s what to try next:
- Physical therapy: Especially for back or knee pain. Manual therapy beats TENS in long-term studies.
- Heat or cold packs: Simple, cheap, and effective for muscle spasms or joint swelling.
- Mind-body techniques: Meditation, breathing exercises, and biofeedback help retrain how your brain processes pain.
- Acupuncture: Works similarly to low-frequency TENS - triggers endorphins and modulates nerve signals.
If your pain is getting worse, or you’re relying on TENS just to get through the day, talk to a pain specialist. TENS is a tool, not a solution. It’s part of a bigger plan.
Final Thoughts: Is TENS Worth It?
Yes - if you use it right.
It’s not a cure. It’s not a replacement for medical care. But for acute flare-ups, post-op recovery, or managing arthritis without pills, it’s one of the most practical, safe, and affordable tools you can buy. It’s portable. You can use it at work, on the couch, or even while walking. No prescriptions. No side effects. No addiction risk.
Just make sure you’re not setting it too low. Don’t treat it like a massage wand. Turn it up until you feel it. And if you’re still not sure, ask a physical therapist. A few minutes of expert guidance could mean the difference between relief and frustration.
Can TENS therapy help with nerve pain?
Yes, but only if the nerve pain is localized - like sciatica or post-surgical nerve irritation. For widespread nerve damage, like diabetic neuropathy, results are mixed. Success depends on precise electrode placement over the affected nerve pathway. Low-frequency TENS (2-5 Hz) is usually better for nerve pain because it triggers natural painkillers. High-frequency may just cause tingling without real relief.
Is TENS safe to use every day?
Yes, for most people. TENS is non-invasive and doesn’t involve chemicals, so daily use is generally safe. Limit sessions to 30-60 minutes at a time, and give your skin a break between uses to avoid irritation. Avoid using it over broken skin, open wounds, or near the eyes, throat, or front of the neck. If you have a pacemaker or other implanted device, talk to your doctor first - electrical pulses can interfere with some medical implants.
Why does my TENS unit stop working after 90 minutes?
It’s likely the battery. Most consumer TENS units run on rechargeable or AA batteries. When you crank the intensity up to get relief, the device draws more power - draining the battery faster. At high settings, 90 minutes is normal. To extend battery life, use lower intensity when possible, or switch to a unit with a larger, rechargeable battery. Some professional models last 10+ hours at full power.
Can I use TENS while sleeping?
No. You shouldn’t use TENS while asleep. You won’t be able to adjust the intensity if it becomes uncomfortable, and there’s a risk of skin irritation or burns from prolonged contact. Also, your body’s natural pain signals might be suppressed during sleep, making it harder to know if the device is working properly. Use TENS during waking hours when you can monitor how you feel.
Do I need a prescription for a TENS machine?
In the U.S., you don’t need a prescription to buy a TENS unit - they’re sold over the counter. But if you want insurance to cover the cost (like Medicare or private plans), you’ll need a prescription and documentation that it’s medically necessary. The Medicare reimbursement code is E0720, and as of 2023, it pays around $150 for a qualifying device. Always check with your provider before buying.
Can TENS therapy replace pain medication?
For some people, yes - especially those managing chronic pain without addiction risks. Many users reduce their reliance on NSAIDs or opioids after using TENS regularly. But it’s not a full replacement. TENS works best as part of a broader plan: physical therapy, movement, stress management, and sometimes medication. Don’t stop your meds without talking to your doctor. TENS is a tool to reduce, not eliminate, the need for drugs.
TENS is just another Western fad dressed up as science. In India, we’ve had Ayurveda and acupressure for 5,000 years-no batteries needed. This gadget is overpriced placebo magic.
I used one after my knee surgery and it worked great until the electrodes fell off every time I moved. Why do these things cost $150 and still use glue that can’t hold a Band-Aid? Also my skin turned red like I got sunburned from a toaster. Not worth it.
Let’s be honest: this is just a glorified tingler. The Gate Control Theory is 60 years old. If you’re relying on this instead of proper rehab, you’re not managing pain-you’re avoiding it. Real progress requires movement, not electricity.
I’ve been using TENS for chronic lower back pain for 3 years now. It’s not a cure, but it lets me play with my kids without crying. The key? Don’t cheap out. Got a dual-channel Omron with conductive gel-life changer. Also, use it while watching Netflix, not just when you’re in agony.
There’s something deeply human about using your own body’s chemistry to heal-endorphins released by TENS feel more like a gift than a pill. It’s not magic, but it’s gentle. Like whispering to your nerves instead of shouting at them with drugs. I wish more doctors understood this.
Just got my first TENS unit!! 😍 Used it for 20 mins while working and my sciatica eased up so much I cried 😭 Thank you for this post-finally something that doesn’t make me feel like a drug addict just for needing relief 🙏
Regarding impedance mismatch and skin-electrode coupling: the 63% signal loss from dry skin is well-documented in IEEE Transactions on Biomedical Engineering (2018). Conductive hydrogel reduces impedance from >10kΩ to <2kΩ, enabling more efficient depolarization of A-delta fibers. Also-burst mode modulates mu-opioid receptor engagement via temporal summation. Not all devices are created equal.
Before you buy a TENS unit, consult a licensed physical therapist. Most users fail because they self-prescribe settings without understanding neurophysiology. A single 30-minute session can triple your success rate. This isn’t a gadget-it’s a clinical tool. Treat it like one.
And yet, despite the FDA clearance, the CDC endorsement, and the Cochrane Review, some people still insist it’s a scam. I’ve seen it work on veterans with phantom limb pain-people who were on 120mg of oxycodone daily, now down to 10mg. If you don’t believe in TENS, you don’t believe in neurology. Or you’re just too lazy to try it right.