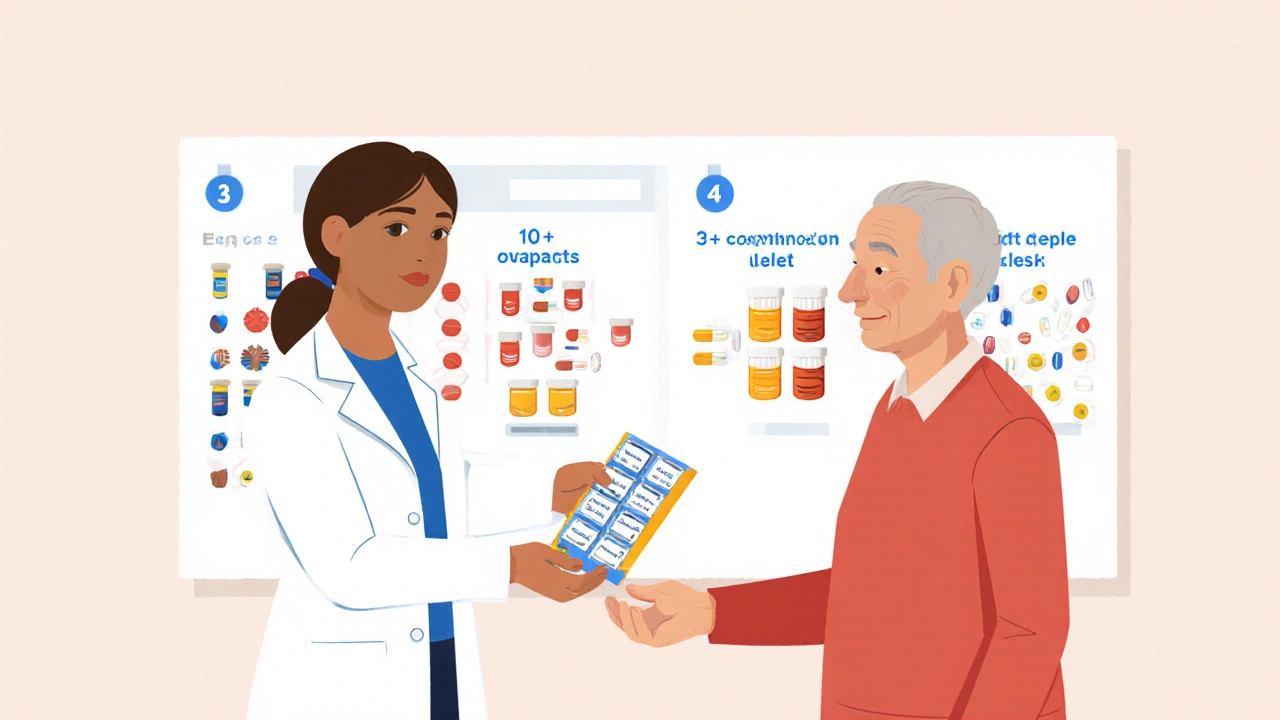
For many older adults, taking medication isn’t just a chore-it’s a full-time job. Imagine waking up to a handful of pills, then repeating the same routine at lunch, dinner, and bedtime. Some seniors swallow eight, ten, even twelve pills a day. That’s not just inconvenient. It’s dangerous. The more pills you take, the more likely you are to forget one, mix them up, or stop taking them altogether. This is called pill burden, and it’s one of the biggest hidden problems in senior healthcare.
What Is Pill Burden, and Why Does It Matter?
Pill burden is the total number of pills a person takes each day. It’s not just about quantity-it’s about complexity. Different times of day, different foods to avoid, varying dosages, multiple pharmacies, refill schedules. It’s overwhelming. And for seniors, especially those with memory issues or arthritis, it’s a recipe for mistakes. The results are serious. Studies show that when people take more than five medications daily, their chance of missing a dose jumps by nearly 50%. Missed doses mean uncontrolled blood pressure, unstable blood sugar, or worsening heart failure. In the long run, this leads to more hospital visits, emergency rooms, and even premature death. The good news? There’s a simple fix that doctors have known about for years but don’t always use: combination medications.How Combination Medications Work
A combination medication-also called a fixed-dose combination (FDC) or single-pill combination (SPC)-is one tablet that contains two or more drugs in a single dose. Instead of taking two pills for high blood pressure, you take one. Instead of three pills for diabetes and cholesterol, you take two. These aren’t new. They’ve been around since the 2000s, but their use has exploded in recent years, especially for chronic conditions like hypertension, heart disease, and type 2 diabetes. For example, a common combination pill might include amlodipine and lisinopril-two separate blood pressure drugs-packed into one tablet. Another might combine metformin and sitagliptin for diabetes control. The science is clear: when you reduce the number of pills, people take them. A major 2007 study in the American Journal of Medicine found that patients using combination pills were 26% more likely to stick to their regimen than those taking the same drugs separately. That’s not a small gain. That’s life-changing.Why Combination Pills Work Better
It’s not magic. It’s psychology and biology working together. First, fewer pills mean less mental load. Your brain doesn’t have to remember which pill goes when. No more confusing red capsules with blue ones. No more wondering if you already took your afternoon pill. Second, fewer pills mean fewer chances for side effects from mismanagement. Taking a diuretic too late in the day? You might wake up every two hours to use the bathroom. Taking a statin without food? Stomach upset. Combination pills often come with optimized timing built in-like a blood pressure pill designed to be taken in the morning, so it works all day without disrupting sleep. Third, there’s a cost benefit. While a combination pill might cost more upfront, it often reduces total out-of-pocket expenses. Fewer prescriptions mean fewer co-pays. Fewer missed doses mean fewer hospital stays. A 2023 analysis in the Journal of Health Economics and Outcomes Research found that combination therapies saved money across the board-for patients, insurers, and the healthcare system.Real-World Impact: Blood Pressure and Beyond
Hypertension is the poster child for combination pills. Nearly 1.3 billion people worldwide have high blood pressure, and most need at least two drugs to get it under control. Yet only about half of patients stick with their regimen. A 2022 review in the European Journal of Cardiology Practice looked at over 80 studies. The result? Patients on single-pill combinations had significantly better blood pressure control. On average, systolic pressure dropped by almost 4 mmHg more than those on separate pills. That might sound small, but in real terms, it means 20% fewer heart attacks and strokes over five years. It’s not just blood pressure. Combination pills are now used for:- HIV (three drugs in one tablet to prevent resistance)
- Tuberculosis (multiple antibiotics in one pill to complete treatment)
- Diabetes and cholesterol (metformin + statin combinations in development)
- Depression and anxiety (some newer combinations target multiple neurotransmitters)
When Combination Pills Don’t Work
Combination pills aren’t perfect. They’re not a one-size-fits-all solution. The biggest downside? Rigidity. Once you’re on a combination pill, you can’t easily adjust the dose of one drug without changing the whole pill. If your blood pressure drops too low on a 10/20 mg combo, you can’t just cut the amlodipine dose in half-you have to switch to a different pill or go back to separate medications. That’s why doctors usually start with individual drugs first. If a patient responds well to one medication but needs a second, then-and only then-do they consider a combination. This avoids overtreating someone who might do fine on just one pill. Also, not all combinations are created equal. Some pills combine drugs with very different half-lives, which can cause uneven effects. Always ask your pharmacist: “Is this combination stable? Do the ingredients work well together?” And if you have allergies, kidney problems, or liver issues, a combination pill might not be safe. A drug that’s fine alone might become risky when mixed. Always review your full list of medications with your doctor before switching.How to Talk to Your Doctor About Combination Pills
Don’t wait for your doctor to bring it up. Ask. Here’s how:- “I’m having trouble keeping track of all my pills. Are there any combination options for my medications?”
- “I’ve been forgetting doses. Would a single-pill combo help me stay on track?”
- “I’m paying a lot in co-pays. Could a combination pill save me money in the long run?”
What to Look for in a Combination Pill
Not all combo pills are the same. Here’s what to check:- Dosage strength: Make sure the dose of each drug is appropriate for you. A 5/10 mg combo might be too strong if you’re just starting out.
- Frequency: Is it once a day? That’s ideal. Twice-daily combos offer less benefit.
- Side effects: Ask if the combo increases the risk of dizziness, fatigue, or swelling compared to taking the drugs separately.
- Insurance coverage: Some combos are more expensive. Ask if there’s a generic version or patient assistance program.

What Comes Next? The Future of Pill Burden
The next wave is the “polypill”-a single tablet with three or more medications. Some are already in trials for heart disease, combining a statin, a blood pressure drug, and aspirin. Early results show promise: patients on polypills were 30% more likely to stick with treatment than those on multiple pills. Technology is helping too. Smart pill dispensers, app-based reminders, and pharmacy delivery services all reduce burden. But nothing works as well as a simple, well-designed combination pill. The goal isn’t just to take fewer pills. It’s to live better. To sleep through the night. To remember your appointments. To feel in control again.Frequently Asked Questions
Are combination medications safe for seniors?
Yes, when prescribed correctly. Combination medications are rigorously tested to ensure the drugs work well together and don’t increase side effects. Doctors check for interactions with other medications, kidney and liver function, and individual health needs before prescribing them. Always review your full medication list with your pharmacist or doctor before switching.
Can I split a combination pill if the dose is too high?
Never split a combination pill unless your doctor or pharmacist says it’s safe. Some pills are designed to release medication slowly, and splitting them can cause dangerous spikes in drug levels. Others have coatings that prevent stomach upset-breaking them can ruin that protection. Always ask before cutting any pill.
Do combination pills cost more than taking separate pills?
Sometimes they do upfront, but often they save money over time. You pay for fewer prescriptions, fewer co-pays, and fewer trips to the pharmacy. More importantly, better adherence reduces hospital visits and emergency care, which can save thousands per year. Ask your pharmacist to compare the total cost of your current regimen versus a combo option.
What if I need to change the dose of one drug in the combination?
If your condition changes-like your blood pressure dropping too low or your kidney function declining-you may need to switch back to individual medications. That’s normal. Combination pills are meant to simplify stable regimens, not to lock you into one dose forever. Your doctor will adjust your treatment plan as needed.
How do I know if a combination pill is right for me?
Ask yourself: Are you forgetting doses? Do you have trouble opening bottles or swallowing multiple pills? Are you paying a lot in co-pays? If you answered yes to any of these, a combination pill could help. Talk to your doctor or pharmacist. They’ll look at your medical history, current medications, and goals to decide if it’s a good fit.
Next Steps for Seniors and Caregivers
Start with a medication review. Grab all your pills-prescription, over-the-counter, vitamins-and bring them to your next doctor or pharmacist visit. Ask:- Which of these can be combined?
- Which ones can I stop safely?
- Is there a once-daily option?


Let’s be real - this whole ‘combination pill’ thing is just Big Pharma’s way to lock you in. They don’t care if you live or die, they care if you stay on their $800/month combo for life. One pill? Sure. But what if you need to tweak one component? You’re stuck. They profit from dependency, not health. And don’t get me started on how they bury the side effect data in footnotes written in Comic Sans.
This is the most important thing you’ll read this year. Fewer pills = fewer mistakes = more living. I’ve seen my grandma forget half her meds until we switched her to three combos. She started sleeping through the night, remembered birthdays, even started gardening again. This isn’t science - it’s dignity. Do it.
As a geriatric pharmacist with 18 years in this field, I can tell you - combination pills are the single most underutilized tool in senior care. The data is overwhelming: adherence jumps 25-30%, hospitalizations drop 40%, and patients report feeling less overwhelmed. But here’s the kicker - most prescribers don’t even ask. They default to prescribing individual meds because it’s easier for them. It’s not laziness - it’s systemic failure. Ask your doctor for a med review. Bring all your bottles. Don’t wait for them to lead. You’re the CEO of your own health. And yes, generics exist for most combos - ask for them. You’re not being difficult - you’re being smart.
Oh wow, another ‘solution’ from people who’ve never held a pill bottle. My uncle took one of these ‘combo’ pills and ended up in the ER because his kidney values went nuclear. No one told him the combo had a diuretic AND an ACE inhibitor. He was 78. They didn’t even check his labs. This isn’t progress - it’s pharmaceutical roulette. And now we’re supposed to cheer? 🤡
Isn’t it ironic? We’ve reduced pill burden by merging drugs… but now we’ve merged our autonomy into a single, unmodifiable tablet. We’re not patients - we’re algorithmic inputs in a corporate wellness dashboard. The real solution isn’t fewer pills. It’s fewer prescriptions. It’s systemic change. It’s rethinking why we’re on so many drugs in the first place. But no - let’s just slap a sticker on the problem and call it innovation.
I’ve been on a combo for blood pressure and statin for five years. It’s the only thing that kept me alive after my second heart attack. I used to take seven pills. Now I take one. I sleep better. I don’t panic when I travel. I don’t need a spreadsheet to remember which blue pill goes with which meal. People say it’s rigid - sure. But sometimes rigidity saves your life. You want flexibility? Try dying from a missed dose. I’ve been there. This isn’t a corporate gimmick. It’s a lifeline.
EVERYTHING ABOUT THIS IS A COVER-UP 🕵️♀️💊 The FDA approves these combos because the drug companies fund their ‘research’ - you think they’d let a pill that saves lives get approved if it didn’t also make them billions? And don’t get me started on the ‘polypill’ - that’s the next step toward mandatory daily medication implants. They’re already testing microchips in pills. You think this is about health? Nah. It’s about control. 🌐👁️ #PharmaControl #WakeUp
Oh my god I’m so glad someone finally said this. My mom was on 11 pills. 11. She’d cry every night because she couldn’t remember which was which. We switched her to four combos. She started singing again. She called me last week and said, ‘I feel like myself.’ That’s not a pill - that’s a miracle. Stop overthinking it. If it works - use it. End of story. 💪❤️
you know what i dont get why do we even need so many pills in the first place like why not just eat better or exercise or something like why are we so lazy as a society to just take a pill for everything like i swear if i had to take one more pill i would just quit living
Combination pills are the epitome of Western medical reductionism - we don’t treat the person, we treat the biomarker. We don’t heal, we optimize. We don’t listen, we prescribe. The real pill burden isn’t the number of tablets - it’s the belief that health can be quantified, packaged, and sold. You want freedom? Stop asking for better pills. Start asking why you need pills at all.
I just wanted to say thank you for writing this. My husband has dementia and we’re drowning in meds. I didn’t even know combination pills were an option until I read this. I’m taking his list to his doctor tomorrow. I’m scared, but also… hopeful. For the first time in months, I feel like there’s a path forward. Not perfect, but better. Thank you.
YEAH RIGHT. COMBO PILLS. THAT’S WHAT THEY WANT YOU TO THINK. MY COUSIN TOOK ONE OF THOSE AND HIS LIVER GOT FRIED. AND NOW HE’S ON ANOTHER 6 PILLS TO FIX THE FIRST ONE. THIS ISN’T HELPING. THIS IS A SCAM. THEY MAKE MONEY OFF THE SIDE EFFECTS TOO. YOU THINK THEY CARE ABOUT YOU? THEY CARE ABOUT YOUR INSURANCE NUMBERS. STOP BEING A SHEEP. 🐑💣