When you pick up a prescription at the pharmacy, you might not realize that your state government had a hand in deciding whether you get the brand-name drug or the cheaper generic version. Across the U.S., states have quietly built a system of rules and financial nudges to push doctors, pharmacists, and patients toward generics. It’s not about forcing anyone-it’s about making the smart choice the easiest one.
Why States Care About Generic Drugs
Generic drugs are chemically identical to their brand-name counterparts but cost 80% to 85% less. In 2023, generics made up 90% of all prescriptions filled in the U.S., but they accounted for only 20% of total drug spending. That gap is why states are so focused on increasing their use. Medicaid, which covers nearly 80 million Americans, spends billions on prescriptions every year. States manage their own Medicaid programs, and drug costs are one of the biggest budget pressures. By steering patients toward generics, states save money without sacrificing health outcomes. A 2018 NIH study found that switching just one in ten brand-name prescriptions to a generic could save states over $50 billion annually.How States Make Generics the Default Choice
States use three main tools to encourage generic use: preferred drug lists, pharmacist substitution rules, and copay differentials. Preferred Drug Lists (PDLs) are the most common tool. Almost every state (46 out of 50) uses them. These are lists of drugs that Medicaid will cover with the lowest out-of-pocket cost. If your doctor prescribes a drug not on the list, you or your doctor must jump through extra hoops-like filling out paperwork or proving the generic won’t work for you. That’s called prior authorization. It’s not a ban, but it’s a strong nudge. Some states review their lists every quarter. Others do it yearly. The goal is to keep the list updated with the cheapest, most effective options. If a new generic hits the market, states want it on the list fast. If a brand-name drug gets a price hike, it gets kicked off.Pharmacist Substitution: The Quiet Game-Changer
Here’s where things get interesting. In most states, your pharmacist can swap a brand-name drug for a generic without asking you. That’s called presumed consent. It’s automatic. You show up for your prescription, and the pharmacist gives you the generic unless you say no. In 11 states, pharmacists must ask you first. That’s explicit consent. The NIH study found a clear difference: states with presumed consent saw generic dispensing rates jump by 3.2 percentage points compared to states that required patient permission. That might sound small, but in a state with 10 million prescriptions a year, that’s 320,000 more generics filled. Why does this work? Because people rarely say no. Most patients don’t know the difference between brand and generic. They trust their pharmacist. And if the price is lower, they’re happy.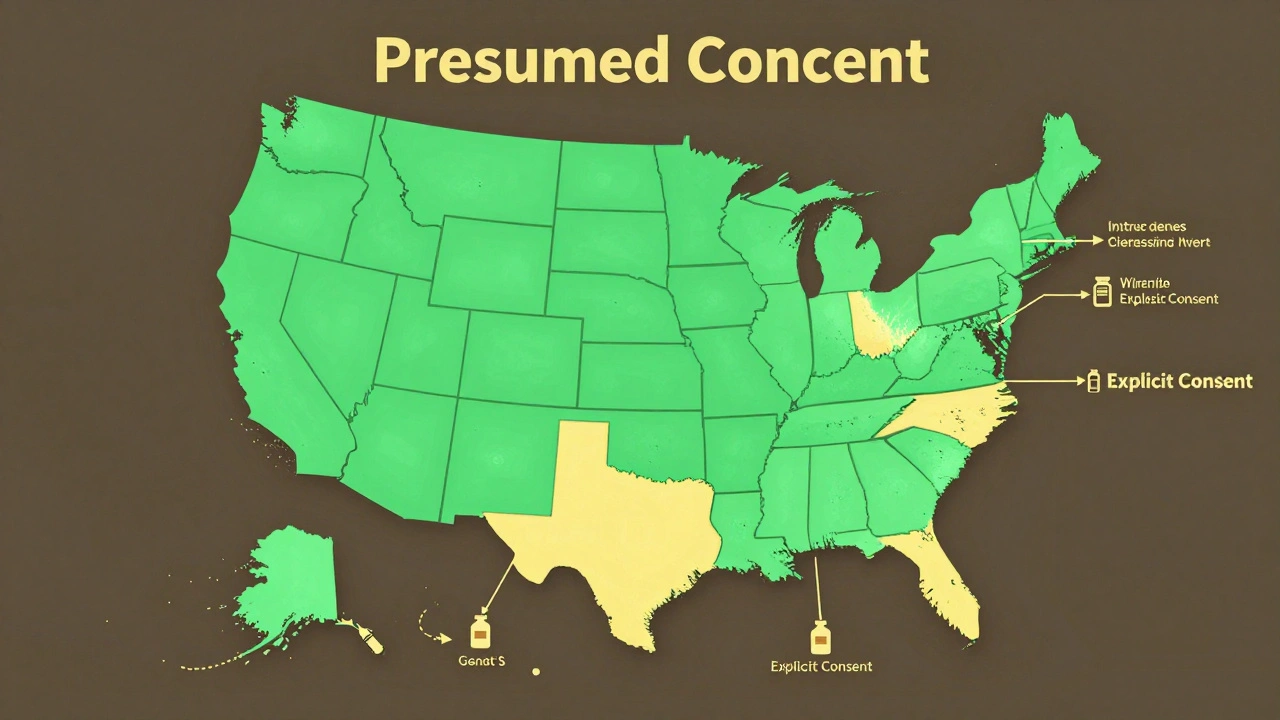
Money Talks: Copay Differences
Another big lever is how much you pay at the counter. States set different copay amounts for brand-name and generic drugs. In many Medicaid programs, a generic might cost $5, while the brand-name version costs $30 or more. This isn’t just about fairness-it’s about behavior. People are more likely to stick with a medication if it’s affordable. A $25 difference can mean skipping a refill. That’s why states focus on closing the gap between what patients pay for brand vs. generic. Back in the late 1990s, pharmacies made almost the same profit on brand and generic drugs-just 8 cents more per generic. But copay differentials kept growing. Today, in many states, the out-of-pocket cost for a generic is so low that patients choose it without thinking.What Doesn’t Work
Not all policies have the same effect. Some states tried mandatory substitution laws-requiring pharmacists to switch every time. But those didn’t move the needle much. Why? Pharmacists were already substituting generics anyway because they made more money on them. The law didn’t change behavior-it just added paperwork. Another misstep? Trying to force doctors to prescribe only generics. Doctors don’t like being told what to write. And if a patient has a rare condition or a bad reaction to a generic filler, a blanket rule can hurt care. The most effective policies are the ones that make the patient the decision-maker-not the doctor or pharmacist. Lower copays, automatic substitution, and clear labeling do more than any mandate.The Hidden Cost: When Generics Disappear
There’s a dark side to these savings. States rely on the Medicaid Drug Rebate Program, which requires drugmakers to pay back a percentage of the drug’s price. For generics, that’s at least 13%. But here’s the catch: if a generic manufacturer’s costs go up-due to supply chain issues, raw material shortages, or inflation-they still have to pay the same rebate. That can make selling a generic in Medicaid unprofitable. A 2022 Avalere Health report found five scenarios where this happens. In some cases, manufacturers have pulled generics off the market entirely. That’s when patients are stuck with expensive brand-name drugs-or no drug at all. It’s a paradox: the very system designed to save money can break the supply of cheap drugs.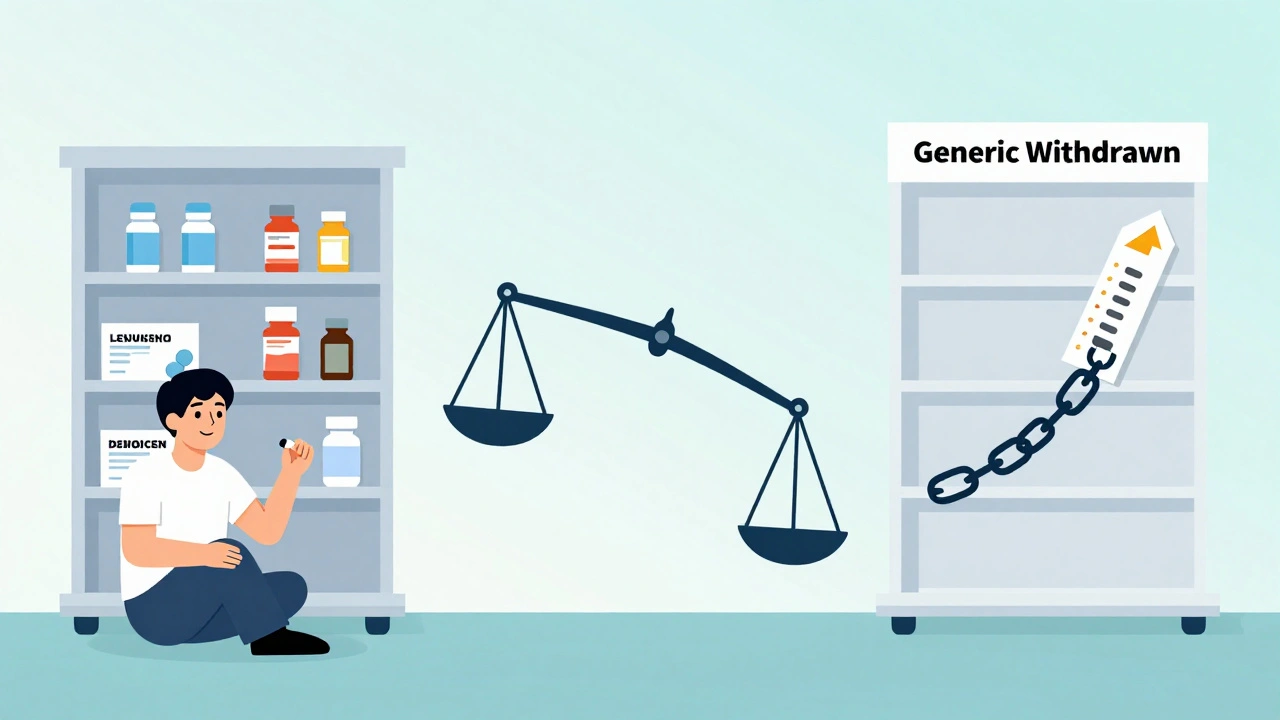
What’s Next? The Drug List
The federal government is watching. CMS, the agency that runs Medicare, is testing a new idea: a $2 Drug List for Part D beneficiaries. It would cap the cost of the most common generics at $2 per prescription-no matter what state you live in. It’s still in development, but if it works, states might copy it. Imagine a list of 50 common generics-metformin, lisinopril, atorvastatin-all costing $2. No copay tiers. No prior authorizations. Just a simple, predictable price. That could be the next big shift: moving from complex state-by-state rules to a national standard for low-cost drugs.What This Means for You
If you’re on Medicaid, your state’s rules directly affect what you pay. Ask your pharmacist: Is there a generic version? Is it on my plan’s preferred list? If you’re paying more than $10 for a common generic, you might be eligible for a cheaper option. If you’re a patient with private insurance, check your plan’s formulary. Many employers and insurers now use the same preferred drug list models as Medicaid. And if you’re a prescriber, know that your state’s rules are designed to help-not hinder. A generic isn’t a compromise. It’s the standard of care.Why This Matters Beyond the Pharmacy Counter
Generic drug policies aren’t just about saving money. They’re about access. When a medication is affordable, people take it. When they take it, their conditions improve. When their conditions improve, hospital visits drop. It’s a chain reaction. States that got this right-like those with presumed consent and low copays-have seen better adherence rates, fewer emergency room visits, and lower overall healthcare costs. The real win isn’t the $50 billion saved. It’s the millions of people who can afford to stay healthy.Do generic drugs work as well as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also meet the same strict standards for quality, safety, and effectiveness. The only differences are in inactive ingredients (like fillers or dyes) and packaging. For over 90% of prescriptions, generics are just as safe and effective.
Can my pharmacist switch my brand-name drug to a generic without asking me?
It depends on your state. In 39 states, pharmacists can substitute generics automatically under "presumed consent" laws-you only get the brand if you ask for it. In 11 states, they must ask you first ("explicit consent"). Check your state’s pharmacy board website or ask your pharmacist to confirm the rules where you live.
Why is my generic drug sometimes more expensive than the brand?
This usually happens because of how insurance or Medicaid calculates reimbursement. Some states use a Maximum Allowable Cost (MAC) list to set the highest price they’ll pay for a generic. If the brand-name drug is discounted heavily or has a rebate, its out-of-pocket cost might be lower than the MAC price for the generic. Always ask your pharmacist to compare the actual cash price before filling the prescription.
Are there any risks to using generic drugs?
For most people, no. But in rare cases, people with severe allergies or sensitivities might react to inactive ingredients in a specific generic version. If you notice a change in how you feel after switching-like new side effects or reduced effectiveness-tell your doctor. They can request the brand or try a different generic manufacturer.
Why do some states have fewer generic incentives than others?
It comes down to politics, budget priorities, and pharmaceutical lobbying. States with strong Medicaid programs and higher drug costs tend to adopt more aggressive policies. States with weaker public health infrastructure or strong ties to drug manufacturers may delay or avoid these measures. But the trend is clear: more states are moving toward presumed consent and lower copays because the savings are real and measurable.

It’s wild how much of our healthcare is shaped by invisible rules. I never thought about pharmacists being able to swap out my meds without asking-until I got a generic I didn’t recognize and had to call my doctor. Turns out, it’s the same stuff. I just didn’t know because no one ever explained it. Now I ask every time, and honestly? I save like $20 a month. Not life-changing, but enough to buy coffee without guilt.
Also, the part about manufacturers pulling generics because of rebates? That’s the kind of systemic irony that keeps me up at night. We’re punishing the cheap solution because the system’s rigged to favor complexity. It’s like trying to fix traffic by adding more toll booths.
It is, without question, an abject failure of governance to permit the substitution of pharmaceuticals without explicit patient consent. The sanctity of informed choice is not a suggestion-it is a constitutional imperative, even if the patient is illiterate, apathetic, or unaware. The state’s paternalism, cloaked in fiscal pragmatism, is a slippery slope toward medical autocracy. One day, they will decide which antidepressants you are permitted to take. And you will thank them for it.
Wait-so the government is secretly manipulating our prescriptions?! And we’re supposed to be grateful?!! This isn’t ‘nudging’-this is coercion wrapped in a spreadsheet!! Who’s really behind these ‘preferred drug lists’?!! Big Pharma?!! Medicaid contractors?!! The same people who price-gouged insulin for decades?!! This is a Trojan horse!!
And don’t get me started on the ‘$2 drug list’-that’s just the first step before they start rationing everything. Next thing you know, they’ll be giving us ‘approved’ painkillers and charging extra for ‘premium’ generics!!
They told us generics were safe. But what if they’re not? What if the fillers are different? What if the FDA doesn’t test them properly?!! Who’s auditing the auditors?!?!?!?!?
generic drugs work fine for most people. i’ve been on them for years. but sometimes they make me feel weird. like, not sick, but off. not sure why. maybe its the dye or something. my doc says its fine, but i still notice a difference. so dont tell me its all the same. people need to know their body reacts different. and if the state makes you take it? thats not helping. its forcing.
also why is my generic more expensive than the brand? that makes no sense. pharmacy lied to me. i felt dumb.
The structural economics here are fascinating. The Medicaid Drug Rebate Program was designed as a cost-containment mechanism, but it’s created a perverse incentive structure where the marginal cost of generic production is decoupled from reimbursement viability. When raw material inflation hits-and it has, consistently since 2020-the rebate floor becomes a ceiling on profitability.
What we’re seeing isn’t market failure-it’s regulatory misalignment. The 13% rebate was calculated on 2006 price points. Today, with global supply chain fragmentation and API sourcing concentrated in two countries, the cost curve has shifted. The policy hasn’t. And that’s why we’re seeing supply collapses in low-margin, high-volume generics-metformin, levothyroxine, hydrochlorothiazide.
We need dynamic rebates tied to input costs, not fixed percentages. Otherwise, we’re just trading short-term savings for long-term access crises.
It’s amusing how the author frames this as ‘patient empowerment’ when, in reality, it’s a carefully engineered behavioral nudge designed to exploit cognitive inertia. The ‘presumed consent’ model doesn’t respect autonomy-it assumes ignorance and capitalizes on it. The fact that patients rarely say no isn’t a triumph of public health-it’s a failure of health literacy.
And let’s not pretend that copay differentials are about affordability. They’re about compliance. The state isn’t trying to make healthcare accessible-it’s trying to make it predictable. To them, patients are variables in a cost-model, not human beings with complex physiological responses.
The ‘$2 Drug List’? A band-aid on a hemorrhage. It doesn’t address the root: a pharmaceutical oligopoly that profits from opacity. Until we break that, all these policies are just rearranging deck chairs on the Titanic.
I’ve worked in community pharmacies for 18 years. I’ve seen people cry because they couldn’t afford their meds. I’ve seen them choose between insulin and rent. I’ve also seen them stare blankly at the generic bottle and say, ‘Is this the same?’
That’s why I always explain it. Not because I have to. Because I want to. I don’t care if the state says I can swap it automatically. I still ask. Because trust matters more than efficiency.
And when someone says ‘yes, I’ll take the generic’-I feel like I helped. Not because I saved money. Because I gave them back control.
That’s what this is really about. Not dollars. But dignity.
so this is how usa fixing drug prices? 😅
in india we just have one price for all generics. no lists, no forms, no fuss. if you need metformin, you buy it for 5 rupees. no one cares if its brand or generic. everyone knows its same.
but here you need a PHD to understand your own prescription 😂
maybe usa need less rules and more trust?
also why is pharmacist even allowed to switch? that's like waiter changing your order without asking 🤔
There’s something deeply poetic about how we’ve turned healthcare into a labyrinth of incentives and opt-outs. We’ve built a system where the cheapest, most effective option is buried under layers of bureaucracy-yet we call it ‘choice.’
But here’s the quiet truth: we don’t actually want to choose. We want to be guided. We want someone, somewhere, to have already decided what’s best. That’s why presumed consent works. Not because people are passive, but because they’re exhausted.
The real innovation isn’t the $2 drug list-it’s the recognition that dignity doesn’t always live in autonomy. Sometimes, it lives in the quiet relief of not having to fight your own medicine.
Maybe the goal isn’t to make patients smarter. Maybe it’s to make the system simpler. And that’s terrifying to bureaucrats. But beautiful to the people who just want to feel okay.
bro why is everyone acting like this is some revolutionary thing??
my grandma gets her meds for $3 and never even knows what brand they are
she just takes em and lives to 92
stop overthinking it 😴
Generics work. Save money. Done.
I’ve seen too many people skip doses because they can’t afford the copay. I’ve held hands with seniors who whispered, ‘I’ll just wait till next month.’
These policies aren’t perfect-but they’re the closest thing we’ve got to saying, ‘You matter.’ Not as a statistic, not as a budget line, but as someone who deserves to take their pill without choosing between groceries and their heart medication.
It’s not about control. It’s about compassion. And if a little nudge helps someone live longer, quieter, healthier days? Then I’m all for it.
Just make sure the pharmacist still asks. Even if the law doesn’t require it. Sometimes, ‘Are you okay with this?’ is the most powerful thing you can say.
One must interrogate the epistemological underpinnings of this ‘generic supremacy’ narrative. The assumption that chemical equivalence equals therapeutic equivalence is a reductive fallacy rooted in positivist dogma.
Pharmaceuticals are not widgets. They are bioactive agents embedded in complex physiological ecosystems. The excipients-those ‘inert’ fillers-can alter dissolution kinetics, bioavailability, and even gut microbiome modulation.
And yet, we are told to trust the algorithm. The PDL. The MAC. The rebate spreadsheet.
This isn’t public health. It’s pharmacological utilitarianism. And the cost? The erosion of individualized care. The quiet death of clinical nuance.
Do we really want a world where your medication is chosen by a spreadsheet and not a physician?
Interesting how the article romanticizes ‘presumed consent’ as a benevolent nudge, while ignoring the cultural asymmetry of trust in healthcare. In the UK, we’ve had similar systems since the 90s-but we call it ‘default substitution,’ and we’re far more transparent about it.
Here’s the kicker: patients in the UK rarely object-not because they’re passive, but because the NHS has spent decades building trust through consistency, communication, and-crucially-no surprise bills.
What’s missing from this piece? The social contract. You can’t engineer compliance without first cultivating confidence. A $2 drug list might work in theory, but without public buy-in, it’s just another bureaucratic performance.
Also, ‘inert ingredients’ aren’t inert. Ever heard of lactose intolerance? Or FD&C dyes? Nah, me neither-until my cousin had a reaction. Then the system didn’t care. Just ‘switch to another generic.’
So yes, save money. But don’t call it empowerment if you’re silencing questions.