When you take a pill, injection, or inhaler, you expect it to work the same way today as it did when it was made-even if it’s been sitting on a shelf for a year. That’s not luck. It’s stability testing. This isn’t just paperwork. It’s a strict, science-backed process that ensures your medicine won’t break down, lose strength, or turn harmful over time. And at the heart of it all are two non-negotiable factors: temperature and time.
Why Temperature and Time Matter in Stability Testing
Pharmaceutical products don’t live in a lab forever. They get shipped across oceans, stored in warehouses without climate control, left in hot cars, or kept in bathroom cabinets. Stability testing simulates these real-world conditions to find out: When does this drug stop being safe and effective? The answer isn’t guesswork. It’s based on decades of global standards. The most widely accepted rules come from ICH Q1A(R2), a guideline created in 2003 by health agencies in the U.S., Europe, and Japan. These rules define exactly how long and at what temperatures you must test a drug before it can be sold. If you skip this step-or do it wrong-you risk patients getting degraded medicine. In 2022, the FDA issued 27 warning letters to drugmakers specifically because their stability data was incomplete or flawed. One company had to recall 150,000 vials of a generic drug because it didn’t catch aggregation issues at 40°C. That’s not a small mistake. That’s a public health risk.Standard Temperature and Time Conditions
There are three main testing scenarios, each with fixed temperature and humidity levels. These aren’t suggestions. They’re regulatory requirements.- Accelerated testing: 40°C ± 2°C and 75% RH ± 5% RH for 6 months. This is the stress test. It’s designed to speed up degradation so you can predict how the drug will behave over years. If something breaks here, you need to fix it before moving forward.
- Long-term testing: Two options exist. Most companies use 25°C ± 2°C and 60% RH ± 5% RH. But if your product will be sold in hot, humid regions like Southeast Asia or Africa, you use 30°C ± 2°C and 65% RH ± 5% RH. You must collect at least 12 months of data before you can submit your drug for approval in the U.S. (FDA requires this). Europe allows 6 months at submission, but you still need to finish the full 12 months later.
- Intermediate testing: 30°C ± 2°C and 65% RH ± 5% RH for 6 months. You only do this if your accelerated test shows a problem and your long-term test is done at 25°C. It’s a bridge to explain why the drug failed under stress.
Refrigerated products-like insulin or some vaccines-have their own rules. Long-term storage is at 5°C ± 3°C for 12 months. Accelerated testing? Not at 40°C. Instead, it’s 25°C ± 2°C and 60% RH. Why? Because freezing and thawing are bigger threats than heat for these products.
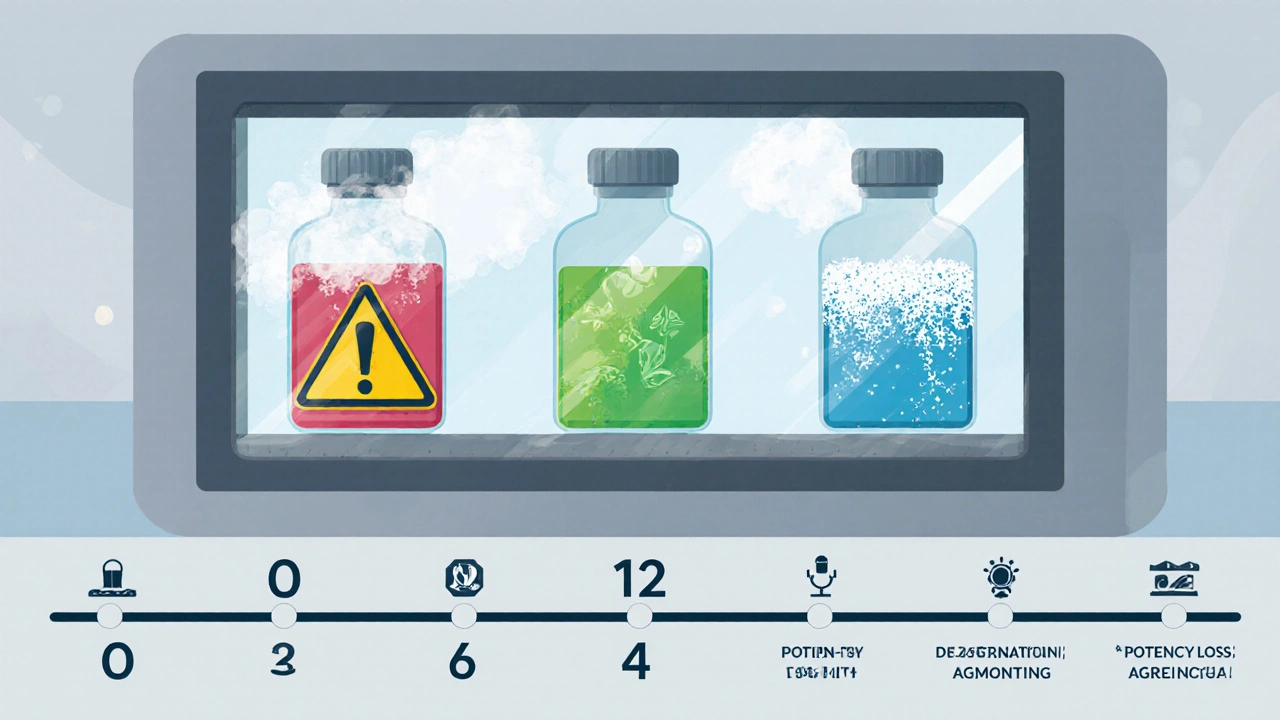
Testing doesn’t happen once. It’s scheduled at 0, 3, 6, 9, 12, 18, 24, and 36 months. Early time points catch quick changes. Later ones confirm long-term stability. And the chambers? They must hold temperature within ±0.5°C and humidity within ±2% RH. Even small drifts can invalidate months of work.
Global Differences and Regional Realities
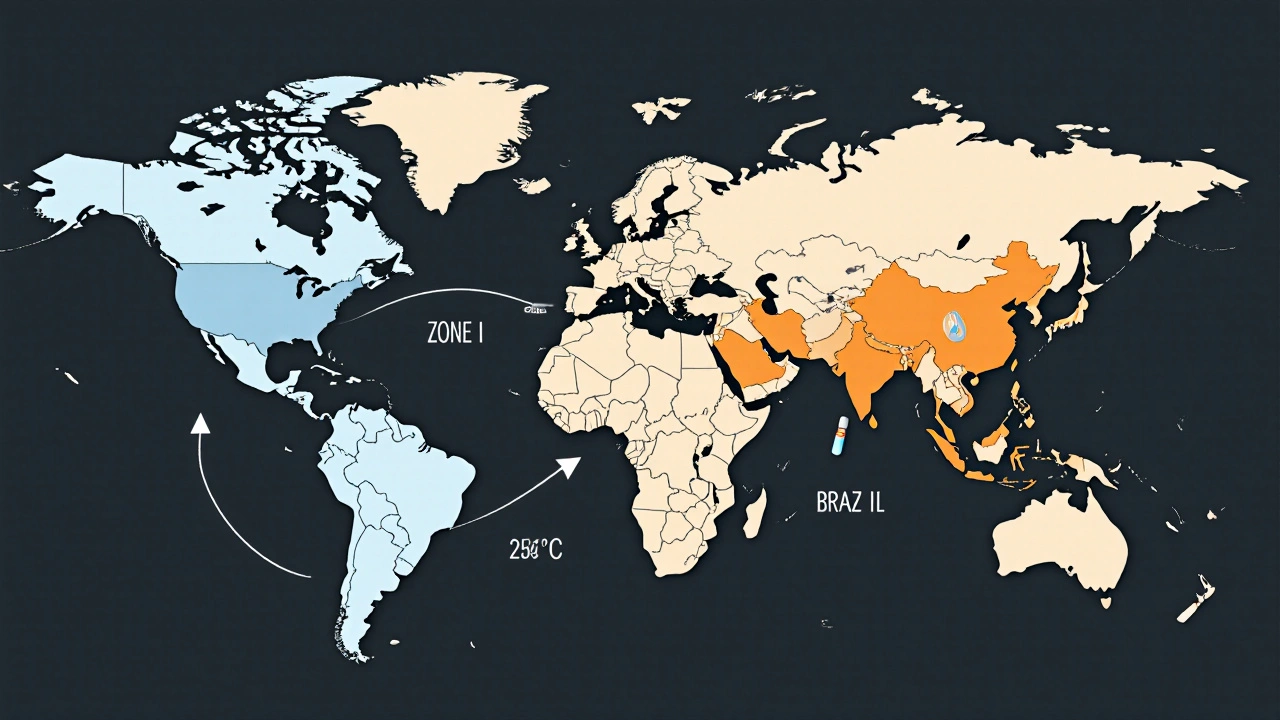
The world isn’t one climate. That’s why ICH created five climatic zones.- Zone I (Temperate): 21°C / 45% RH
- Zone II (Subtropical): 25°C / 60% RH
- Zone III (Hot-Dry): 30°C / 35% RH
- Zone IVa (Hot-Humid): 30°C / 65% RH
- Zone IVb (Hotter, Higher Humidity): 30°C / 75% RH
If you’re selling a drug in India or Brazil, you need to test under Zone IVa conditions. If you’re targeting Australia or Canada, Zone II is enough. But here’s the catch: if you want global approval, you often have to run multiple studies. That adds 4-6 months to development time and increases costs by hundreds of thousands of dollars.
Regulatory agencies don’t always agree. The FDA insists on 12 months of long-term data at submission. The EMA lets you submit with 6 months, but you must finish the full 12 months later. For companies launching worldwide, this creates delays. One drugmaker spent 11 months waiting for EMA approval after FDA clearance-just because their data package didn’t meet both timelines.
What Happens When the Numbers Don’t Add Up
The biggest gray area in stability testing isn’t the temperature. It’s the word “significant change.” ICH Q1A(R2) says you need to report changes in: assay (strength), degradation products, appearance, and dissolution. But it doesn’t say how much change is too much. Is a 3% drop in potency a problem? What about a 5% increase in impurities? The guidelines leave it open. That’s where things get messy. One Pfizer analyst shared a story on Reddit: their drug showed a 4.8% drop in assay. The specification was 95-105%. Statistically, it was fine. But the regulator called it a “significant change” and blocked approval. Why? Because their internal threshold was 5%. The other company? They used 7%. No one told them what the rule was. Just that they had to meet it. This subjectivity causes delays, retests, and sometimes recalls. In 2021, Teva had to pull 150,000 vials because their stability protocol didn’t catch aggregation at 40°C. The same drug, tested under the same conditions by a different lab, passed. That’s not a flaw in the drug. It’s a flaw in how we interpret the data.Real-World Challenges in the Lab
Running stability studies sounds simple: put samples in a box and wait. But it’s anything but.- Temperature excursions happen. A 2023 survey of 142 stability professionals found 78% had at least one chamber spike above ±2°C. One 3-hour power outage can ruin 12 months of work.
- Humidity control is harder than you think. In dry climates like Arizona or Australia, keeping 60% RH requires constant humidification. Without it, tablets can dry out, crack, or lose potency.
- Chambers aren’t uniform. Temperature can vary by ±1.8°C from top shelf to bottom. That’s why every chamber must be mapped before use-every single time.
- Biologics and mRNA vaccines don’t play by the old rules. Freeze-thaw cycles, agitation, and light exposure can destroy them. Standard 40°C tests won’t catch that. Companies are now adding dynamic humidity cycling and vibration tests, but those aren’t in ICH yet.
And then there’s the wait. Stability testing takes years. A new drug can sit in a chamber for 24 months before you know if it’s stable. That delays launches, blocks revenue, and frustrates teams. One company lost $40 million in projected sales because their stability data came in 11 months late.
The Future: Modeling, Automation, and Change
The system works-for traditional pills and injections. But it’s struggling with modern medicines.- Antibody-drug conjugates (ADCs), gene therapies, and lipid nanoparticles degrade in ways ICH never predicted.
- Real-time release testing (RTRT) and process analytical technology (PAT) are making traditional stability studies feel outdated. If you can monitor quality during manufacturing, why wait 12 months to test?
- Companies like Merck and Pfizer are now using predictive models. They test at 50°C, 60°C, even 80°C to simulate years of degradation in weeks. These models are 74% accurate for small molecules-but they still aren’t accepted by regulators.
ICH is working on an update-Q1F-expected in late 2024. It’s supposed to cover complex products and maybe even allow model-based data. But regulators are cautious. In 2022-2023, the EMA rejected 8 submissions that relied entirely on predictive models.
The future isn’t replacing physical testing. It’s combining it. Think of it like this: you still need to drive the car to know it works-but now you can also simulate the crash in a computer first.
What You Need to Get Started
If you’re new to stability testing, here’s what you actually need:- Qualify your chambers. Do IQ/OQ/PQ tests. Don’t skip this. ASTM E1993-19 is the standard.
- Map your chambers. Find hot and cold spots. Adjust shelf placement.
- Choose your test conditions based on your target markets. Don’t assume 25°C is enough.
- Document everything. Protocols, raw data, reports. A typical dossier runs 500 pages.
- Train your team. Stability analysts need stats knowledge, chamber skills, and regulatory writing ability. It takes 6-9 months to become proficient.
Stability testing isn’t glamorous. But it’s the invisible shield between a patient and a dangerous drug. Get it right, and you protect lives. Get it wrong, and you risk everything.
What are the standard temperature and humidity conditions for long-term stability testing?
The two standard conditions are 25°C ± 2°C / 60% RH ± 5% RH and 30°C ± 2°C / 65% RH ± 5% RH. The choice depends on the climatic zone where the product will be sold. The 25°C condition is used for temperate markets like the U.S. and Europe. The 30°C condition is required for hot, humid regions like Southeast Asia and Africa. At least 12 months of data must be collected before regulatory submission in the U.S.
How long does accelerated stability testing last?
Accelerated testing runs for 6 months at 40°C ± 2°C and 75% RH ± 5% RH. This condition is designed to accelerate degradation and predict long-term behavior. If the product shows significant changes during this test, intermediate testing or formulation changes may be needed. The results from accelerated testing are not used to set shelf life-they’re used to identify risks early.
What is the difference between ICH Q1A(R2) and other stability guidelines?
ICH Q1A(R2) is the globally harmonized standard adopted by the FDA, EMA, Health Canada, and other major regulators. It replaced older regional rules, reducing duplicate testing. While other organizations like WHO have supplemental guidelines for refrigerated products or tropical climates, ICH Q1A(R2) remains the core framework. Minor differences exist in submission requirements-for example, the EMA allows 6 months of long-term data at submission, while the FDA requires 12 months.
Why do some stability tests fail even when the product seems fine?
Many failures occur because of subtle changes-like a 4% drop in potency or a small increase in impurities-that regulators classify as “significant change.” The ICH guidelines don’t define exact thresholds, so interpretations vary between agencies and even between labs. A change that seems statistically insignificant to one team may be rejected by a regulator who follows a stricter internal policy. Humidity cycling, not just constant RH, is also a major cause of failure in solid dosage forms, but this isn’t always tested.
Can predictive modeling replace physical stability testing?
Not yet. While predictive models using high-temperature testing (50-80°C) can estimate shelf life faster and are used by 74% of top pharmaceutical companies, regulators still require physical data. The EMA rejected 8 model-based submissions in 2022-2023. The industry is pushing for change, and ICH is working on new guidelines (Q1F) that may allow hybrid approaches. But for now, physical testing remains mandatory for approval.
What are the biggest challenges in running stability studies?
The biggest challenges are chamber reliability, humidity control, and the long wait times. Temperature excursions-even brief ones-can invalidate studies. Humidity control is especially difficult in dry climates. Waiting 12-36 months for data delays product launches and costs millions. Biologics and novel formulations like mRNA vaccines don’t always follow traditional degradation patterns, making standard tests unreliable. Many companies now use dual-loop environmental systems to reduce RH variation from ±8% to ±3%.
This post hit me right in the feels. I work in pharma QA and stability testing is the silent hero no one talks about. You ever see a lab tech staring at a chamber like it’s a baby? That’s not obsession-that’s responsibility. One tiny temp spike and a whole batch of insulin could turn to soup. We lost a shipment last year because a freezer glitched during a storm. No one died, but we cried. And then we fixed the backup system. Again.
YASSS THIS IS WHY WE CAN’T HAVE NICE THINGS 😭
Regulators are literally playing Jenga with people’s lives. One 0.2% impurity spike and suddenly your $200M drug is trash. Meanwhile, some startup in Bangalore is selling fake metformin in a box labeled ‘For External Use Only’ and nobody bats an eye. Double standards? More like triple standards with extra drama.
Also-why is 40°C the magic number? Did someone at ICH just spin a wheel and go ‘yep, that’s hot enough’? 😅
Stability testing is the quiet backbone of modern medicine. We don’t cheer for it like we do for new cancer drugs. But without it, every pill is a gamble. The real tragedy isn’t the 12-month wait-it’s that we still treat it like a checkbox instead of a science. We’ve mapped Mars but still can’t agree on what ‘significant change’ means. Maybe the problem isn’t the data-it’s our fear of nuance.
Just to clarify-ICH Q1A(R2) is the baseline, but regional deviations are a nightmare. For example, if you're submitting to Brazil (Zone IVa), you need 12 months at 30°C/65% RH even if your primary market is the US. And don’t get me started on biologics-mRNA vaccines degrade via different pathways, so standard accelerated testing at 40°C is useless. You need dynamic humidity cycling, light exposure assays, even agitation studies. Most labs aren’t equipped. And yeah, the 0.5°C chamber tolerance? Non-negotiable. One of my colleagues had a 3-hour outage that invalidated 18 months of data. They’re still paying for it.
THEY’RE LYING TO YOU. EVERY SINGLE ONE OF THEM.
Stability testing isn’t about safety-it’s about control. Big Pharma doesn’t want you to know how fragile these drugs really are. That’s why they hide the real thresholds. The 5% potency drop? That’s not a ‘significant change’-it’s a cover-up. The FDA and EMA are in bed with the labs. They’re all part of the same cartel. Why do you think they reject predictive models? Because if you can simulate shelf life in weeks, you don’t need $500k chambers. And if you don’t need chambers, you don’t need them. They’re scared. The truth is out there. Check the FOIA requests. They’re deleting files.
Why do we even do this? So some guy in Ohio can take his blood pressure pill after it sat in a hot car for 3 hours? I mean… it’s fine. I’ve had meds that tasted weird and I lived. Just let people take their chances. Why spend millions to make medicine ‘perfect’? People die from bad food, bad air, bad water-why are pills so sacred? 🤷♀️
So you’re telling me we test drugs at 40°C… but I left my insulin in my car at 38°C and it was fine? Hmm. So… this whole thing is just corporate theater? I’m not impressed. Also, why is the word ‘chamber’ used so much? Sounds like a sci-fi prison. 🙄
Been there. Done that. The chambers are always lying. Map them. Always. I once had a shelf that was 2°C colder than the rest. Took us six months to find it. We thought the drug was degrading. Turns out it was just the shelf. Now I check every drawer like it’s a crime scene. No drama. Just data.
I work with new grad analysts and I see them panic every time a result looks ‘off.’ I tell them: ‘It’s not a failure-it’s a clue.’ Stability testing isn’t about perfection. It’s about understanding. That 4.8% drop? It’s not the end. It’s the start of a conversation. We don’t shut things down-we dig deeper. And if you’re ever tempted to cut corners? Remember: someone’s grandpa is taking that pill. You’re not just running tests. You’re holding a hand.
Love this breakdown! As someone from India, I’ve seen how hard it is to keep meds cool in monsoon season. We need more Zone IVa testing, not less. And yes, predictive modeling is the future-but we can’t rush it. I’ve seen labs in Mumbai use old fridges for long-term studies. No joke. The gap between global standards and real-world conditions is huge. Maybe ICH should include a ‘low-resource’ testing protocol. Not everyone has a ±0.5°C chamber. But everyone needs safe medicine.
Wait. You mean the 12-month requirement isn’t arbitrary? And the 40°C isn’t just a guess? And the chambers need mapping? Wow. I thought this was all just paperwork. My bad. 😅
Thank you for writing this. I’m a new stability analyst and I’ve been drowning in protocols. This made me feel seen. The part about ‘significant change’-I’ve spent hours crying over a 0.3% impurity increase. Turns out, it’s not me. It’s the system. We’re all just trying to do right by patients. Even if the guidelines are messy. Even if the chambers break. We show up. And that matters.
Stability testing? More like stability theater. They test at 40°C but real cars hit 60°C. They test for 12 months but people keep meds in bathrooms for 5 years. This whole thing is a fantasy. Just slap a ‘use within 3 months of opening’ label and be done with it. Nobody reads the fine print anyway.