Anxiety & Acid Indigestion Symptom Tracker
Recent Symptoms
Tip: Patterns often emerge after logging 7-10 days. Note how your anxiety levels correlate with acid indigestion symptoms.
Key Takeaways
- Acid indigestion and anxiety share a two‑way street via the gut‑brain axis.
- Stress hormones, the vagus nerve, and stomach‑acid levels all play a part.
- Changing diet, sleep habits, and stress‑relief techniques can ease both issues.
- If symptoms persist, a doctor can recommend tests, medication, or therapy.
- Keeping a symptom diary helps identify triggers and track progress.
What Is Acid Indigestion?
When acid indigestion a burning or painful sensation in the upper abdomen caused by excess stomach acid refluxing into the esophagus flares up, the first thing most people reach for is an antacid. While occasional heartburn is normal, frequent bouts point to an underlying imbalance in stomach acid hydrochloric acid that helps break down food in the stomach or a weakened lower esophageal sphincter.
Common signs include:
- A burning feeling behind the breastbone (heartburn)
- Bloating, belching, or a sense of fullness
- Nausea or a sour taste in the mouth
These symptoms are often lumped together under the medical term dyspepsia general discomfort in the upper abdomen without a clear cause. When dyspepsia becomes chronic, it may be classified as gastroesophageal reflux disease (GERD).
What Is Anxiety?
Anxiety a mental‑health condition marked by excessive worry, restlessness, and physical tension isn’t just a feeling; it triggers a cascade of physiological changes. The brain’s amygdala flags perceived threats, prompting the hypothalamus to fire up the HPA axis the hypothalamic‑pituitary‑adrenal system that releases cortisol and adrenaline. Those stress hormones prepare the body for “fight or flight,” but they also affect digestion.
Typical anxiety symptoms include:
- Rapid heartbeat or palpitations
- Muscle tension, especially in the neck and jaw
- Sleep disturbances
- Gastro‑intestinal upset (nausea, cramps, or diarrhea)
Notice how the gut shows up again? That overlap is no coincidence.
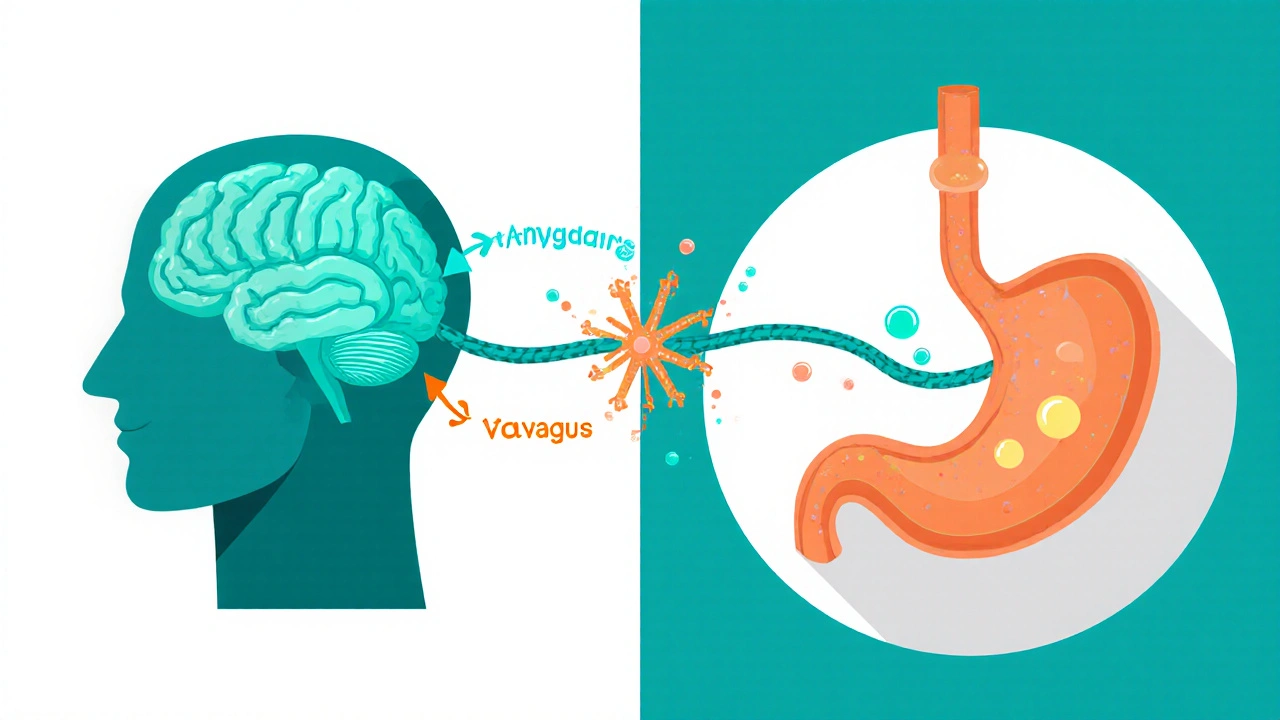
The Gut‑Brain Connection
The gut‑brain axis a bi‑directional communication network linking the central nervous system and the gastrointestinal tract relies on three main channels:
- The vagus nerve - the longest cranial nerve that carries signals both ways.
- Hormonal messengers such as cortisol the primary stress hormone released by the adrenal glands and adrenaline.
- The microbiome - trillions of bacteria that produce neurotransmitters like serotonin a mood‑regulating chemical, about 90% of which is made in the gut.
When the brain signals stress, the vagus nerve can speed up acid production, relax the lower esophageal sphincter, and slow gut motility. Conversely, irritation in the esophagus can send pain signals that heighten the brain’s threat response, feeding anxiety.
How Anxiety Triggers Acid Indigestion
Several mechanisms explain why anxiety often precedes a bout of heartburn:
- Increased acid secretion: Cortisol and adrenaline stimulate the stomach’s parietal cells, leading to more stomach acid hydrochloric acid that aids digestion but can irritate the esophagus when overproduced.
- Relaxed sphincter: Stress hormones relax smooth muscle, including the lower esophageal sphincter, allowing acid to splash back up.
- Altered gut motility: Anxiety can speed up or slow down stomach emptying, causing pressure that pushes acid upward.
- Hyper‑awareness of sensations: An anxious mind often interprets mild heartburn as severe, amplifying the discomfort.
Because the body’s response is automatic, you may feel the burn even if you haven’t eaten a big meal.
How Acid Indigestion Can Heighten Anxiety
When acid irritates the esophageal lining, nerve endings send pain signals to the brain. The brain interprets that pain as a threat, which can trigger a stress response. Over time, recurring pain creates a conditioning loop: the brain expects discomfort, so anxiety spikes even before the next meal.
Other ways the cycle feeds itself:
- Sleep disruption: Night‑time reflux wakes you up, leading to fatigue and increased worry the next day.
- Social avoidance: Fear of experiencing heartburn in public may cause you to skip events, which fuels social anxiety.
- Medication side effects: Some antacids contain calcium carbonate, which in large doses can cause constipation and mood swings, while certain anti‑anxiety drugs (like SSRIs) may aggravate reflux in sensitive individuals.
Breaking this loop requires addressing both the physical and mental sides.
Practical Steps to Break the Cycle
Below is a checklist you can start using today. Treat it like a mini‑program: pick three items, try them for a week, and adjust based on what works.
| Category | Immediate Relief | Long‑Term Habit |
|---|---|---|
| Diet | Chew a piece of ginger or sip warm water with a dash of honey. | Limit caffeine, chocolate, spicy foods, and alcohol; eat smaller meals 2-3 hours before bed. |
| Stress Management | Practice 5‑minute diaphragmatic breathing when you feel a rise in heartburn. | Incorporate daily mindfulness, yoga, or short walks to keep cortisol levels in check. |
| Medication | Take an over‑the‑counter antacid (e.g., calcium carbonate) as directed. | Discuss with a clinician the use of H2‑blockers or proton‑pump inhibitors, especially if reflux is frequent. |
| Sleep | Elevate the head of the bed 6‑8 inches. | Maintain a regular bedtime, avoid late‑night meals, and keep the bedroom cool and dark. |
| Mental Health | Try a brief grounding exercise (5‑4‑3‑2‑1 sensory technique). | Consider cognitive‑behavioral therapy (CBT) or counseling for chronic anxiety. |
In addition, a few probiotics live microorganisms that may improve gut flora balance can support a healthier microbiome, which in turn influences serotonin production.
Track your meals, stress levels, and reflux episodes in a simple spreadsheet. Patterns often emerge-like a spike after a 3 pm coffee or during a deadline crunch.
When to Seek Professional Help
If you notice any of the following, schedule a visit:
- Heartburn that persists beyond two weeks despite OTC treatment.
- Difficulty swallowing, unexplained weight loss, or vomiting.
- Anxiety that interferes with work, relationships, or daily tasks.
- Frequent use of antacids (more than twice a day).
A primary‑care doctor can order an upper endoscopy to rule out esophagitis or Barrett’s esophagus. They may also refer you to a gastroenterologist for specialized testing or to a mental‑health professional for anxiety‑focused therapy.
Putting It All Together
The takeaway is simple: acid indigestion and anxiety are tightly linked through hormones, nerves, and the gut microbiome. By tackling both the physical triggers (diet, sleep, medication) and the mental side (stress reduction, therapy), you can lower the frequency of heartburn and calm the nervous system at the same time.
Start with a symptom diary, try a few lifestyle tweaks, and don’t hesitate to ask a doctor for a deeper look if the pattern sticks. Small changes add up, and over time you’ll likely notice less burning and a calmer mind.
Can anxiety cause heartburn without any food triggers?
Yes. Stress hormones can increase stomach‑acid production and relax the lower esophageal sphincter, leading to reflux even when you haven’t eaten a large or spicy meal.
Do antacids make anxiety worse?
Most over‑the‑counter antacids are neutral, but taking them in excess can cause electrolyte imbalances that affect mood. If you’re on prescription anxiety medication, check with your doctor before using antacids regularly.
Is there a link between probiotics and reduced anxiety?
Research suggests that a balanced gut microbiome can boost serotonin production, which may lower anxiety levels. Strains like Lactobacillus rhamnosus have shown modest benefits in clinical trials.
When should I consider seeing a gastroenterologist?
If heartburn lasts longer than two weeks, you experience difficulty swallowing, or you need antacids daily, a specialist can run an endoscopy and prescribe stronger medications if needed.
Can CBT help with reflux symptoms?
Cognitive‑behavioral therapy targets the anxiety that fuels acid production. Many patients report fewer flare‑ups after learning stress‑management techniques.
Wow, what a tangled dance between the gut and the mind!
If your stomach is on fire, remember you’re not alone-your brain is literally whispering fire alarms.
Try swapping late‑night pizza for a calming ginger tea and do a quick belly‑breathing exercise; you’ll feel the flames die down.
Keep a simple diary, note the stressors, and watch the pattern fade like fog.
You’ve got this, and every small win is a victory worth celebrating!
I feel you bro, that burn can feel like a dragon breathing in your chest.
Small changes like not guzzlin coffee right before bed really help.
Keep tracking, it’s the best way to spot the sneaky triggers.
You’re doing great, just keep at it!
The gut‑brain axis is essentially a two‑way street where chemistry meets cognition, and each fire of anxiety can set off a cascade of acid production.
Think of stress as a signal amplifier that turns a mild rumble into a full‑blown reflux episode.
By calming the central nervous system through mindfulness, you indirectly tell your stomach to dial back the acid.
This feedback loop illustrates how mental health and digestion are inseparably linked, not merely co‑incidental.
Embracing this perspective can empower you to treat both sides simultaneously.
The premise that anxiety fuels acid secretion rests on well‑documented endocrine pathways.
When the hypothalamic‑pituitary‑adrenal axis activates, cortisol surges and directly stimulates parietal cells.
Simultaneously adrenaline induces smooth muscle relaxation, which includes the lower esophageal sphincter.
This physiological combination creates a perfect environment for gastric contents to ascend.
Epidemiological data show a statistically significant overlap between diagnosed generalized anxiety disorder and chronic dyspepsia.
Moreover, functional MRI studies reveal heightened activity in the insular cortex during both stress and esophageal irritation.
The vagus nerve, serving as the primary conduit, transmits afferent signals that the brain interprets as threat, perpetuating the cycle.
Chronically, this loop can condition the central nervous system to anticipate pain, lowering the threshold for anxiety spikes.
Interventions that target either side of the loop, such as cognitive‑behavioral therapy or proton‑pump inhibitors, demonstrate measurable reductions in symptom severity.
Clinical trials also indicate that probiotics modulating the microbiome can attenuate cortisol responses.
From a systems‑theory perspective the gut and brain behave as coupled oscillators whose resonance can be dampened by lifestyle adjustments.
Practical steps like elevating the head of the bed, avoiding late‑night caffeine, and practicing diaphragmatic breathing alter the input parameters of this system.
Long‑term adherence to such practices re‑establishes homeostatic balance and reduces the frequency of reflux episodes.
Therefore the assertion that anxiety is merely a psychological construct divorced from gastrointestinal function is scientifically untenable.
In summary a multidisciplinary approach that respects the bi‑directional communication between mind and gut offers the most robust path to relief.
Implementing a brief diaphragmatic breathing routine before meals can markedly reduce reflux episodes.
It’s unforgivable how many people ignore the warning signs of chronic heartburn, sacrificing their mental peace for the illusion of convenience; we must demand better self‑care, because neglect is a silent betrayal of our own body.
While the article covers the basics, it oversimplifies the role of the microbiome by treating it as a single entity rather than a complex ecosystem; recent metagenomic studies reveal strain‑specific effects on serotonin synthesis that could refine treatment protocols.
Additionally, the recommendation to elevate the head of the bed lacks dosage guidance-how many centimeters is optimal?
A more nuanced discussion would empower readers to tailor interventions rather than follow blanket advice.
To elucidate the mechanistic pathway, one must consider the catecholamine‑mediated modulation of gastric H⁺‑K⁺‑ATPase activity, which is upregulated during acute stress responses; this biochemical cascade is corroborated by controlled laboratory assays utilizing plasma cortisol quantification.
Consequently, any therapeutic regimen that fails to address this endocrine component is fundamentally incomplete.
The interplay between anxiety and acid reflux is a quintessential example of psychosomatic integration, wherein emotional turbulence translates into tangible physiological distress.
From a clinical perspective, it is imperative to adopt a comprehensive assessment strategy that captures both psychological scales and gastroenterological metrics.
Patients reporting episodic heartburn should be prompted to complete a validated anxiety inventory such as the GAD‑7, thereby establishing a baseline for mental health.
Conversely, individuals diagnosed with generalized anxiety disorder ought to undergo esophageal pH monitoring to detect subclinical reflux events.
Empirical evidence indicates that a reduction of at least two points on the anxiety scale correlates with a 30 % decrease in reported reflux severity.
Lifestyle modifications, including the elimination of caffeine after noon, the adoption of a Mediterranean diet rich in omega‑3 fatty acids, and the implementation of nightly mindfulness meditation, have been shown to synergistically attenuate both symptom clusters.
Pharmacologically, the judicious use of a selective serotonin reuptake inhibitor may indirectly modulate gut motility, while a proton‑pump inhibitor addresses the acid component.
It is crucial, however, to monitor for potential drug‑drug interactions, especially considering the metabolic pathways involving CYP450 enzymes.
Regular follow‑up appointments should incorporate diary reviews, allowing clinicians to pinpoint temporal patterns linking stressors to reflux flare‑ups.
Moreover, incorporating biofeedback techniques can empower patients to gain volitional control over autonomic responses that precipitate acid secretion.
The therapeutic alliance between gastroenterologists and mental health professionals should be reinforced through interdisciplinary case conferences.
Such collaboration ensures that treatment plans are not fragmented but rather integrated, addressing the bidirectional nature of the condition.
Patients often find reassurance in understanding that their symptoms are not merely ‘in their heads’ but stem from a legitimate physiological cascade.
Educating patients about the gut‑brain axis demystifies the process and reduces stigma associated with seeking mental health support.
Finally, sustained adherence to the outlined strategies typically yields progressive improvement over a span of weeks to months, illustrating the cumulative benefit of holistic care.
By embracing this multifaceted approach, individuals can reclaim both digestive comfort and psychological tranquility.