When someone overdoses on benzodiazepines, time isn’t just important-it’s everything. These drugs, prescribed for anxiety, insomnia, or seizures, can slow breathing to a dangerous level, especially when mixed with alcohol or opioids. The good news? Isolated benzodiazepine overdoses rarely kill. The bad news? They’re often not isolated. Most fatal cases involve other depressants, and the signs can be easy to miss if you’re not looking for them.
What Happens During a Benzodiazepine Overdose?
Benzodiazepines work by boosting GABA, the brain’s main calming chemical. Too much of it, and your central nervous system shuts down. You don’t usually vomit or convulse like with other overdoses. Instead, you get quiet, deep sedation. Eyes roll back. Breathing gets shallow. Speech slurs. You might look like you’re asleep-but you can’t be woken up. The risk spikes with certain drugs. Alprazolam (Xanax) is 3.2 times more likely to cause intubation than other benzodiazepines. Illicit versions like etizolam and clonazolam are even worse-3 to 10 times more potent. These aren’t pills you get from a pharmacy. They’re pressed into fake Xanax tablets and sold on the street. In the Western U.S., they now cause 68% of severe overdoses.Emergency Response: ABCDE Protocol
There’s no magic antidote. No pill to swallow. The standard is simple: ABCDE.- Airway: Is the person’s airway clear? If they’re unresponsive, tilt the head back and lift the chin. If they’re snoring or gurgling, they need immediate help.
- Breathing: Count breaths. Less than 10 per minute? That’s a red flag. Oxygen comes first-15 liters per minute via a non-rebreather mask. For patients with COPD, switch to a Venturi mask to avoid CO2 buildup.
- Circulation: Check pulse and blood pressure. Heart rate and rhythm should be monitored continuously. ECG is standard.
- Disability: Use the Glasgow Coma Scale. A score of 8 or lower means you need an anesthesiologist now. Don’t wait.
- Exposure: Remove clothes if needed. Look for signs of other drugs-needle marks, pill bottles, empty vials.
What Tests Are Needed?
Don’t assume it’s just benzodiazepines. Over 70% of cases involve other substances. You need to rule out:- Low blood sugar (hypoglycemia)-a quick fingerstick test takes 30 seconds.
- Acetaminophen and aspirin overdose-common in suicide attempts.
- Ethanol (alcohol) levels-often the hidden factor.
- Urine toxicology screen-catches opioids, sedatives, and new synthetic benzos.

Flumazenil: The Antidote That’s Usually the Wrong Choice
Flumazenil reverses benzodiazepines. Sounds perfect, right? It’s not. It’s dangerous. Its half-life is only 41 minutes. That means sedation can return after it wears off, requiring repeat doses. Worse, it can trigger seizures in people who’ve been taking benzodiazepines long-term-even if they’re not addicted, just dependent. That’s a 38% risk, according to StatPearls. And if opioids are involved? Flumazenil won’t touch them. You’ll reverse the benzo, but the person still can’t breathe. The opioid stays. That’s why the American College of Medical Toxicology says flumazenil is appropriate in only 0.7% of cases. Most emergency departments stopped stocking it. Only 12.3% of doctors have ever given it. One Reddit user wrote: “Saw a patient seize 90 seconds after flumazenil-turns out he was on trazodone and alprazolam. No one checked the meds.”Activated Charcoal? Only If Given Fast
Benzodiazepines absorb quickly. If someone took them more than 60 minutes ago, charcoal won’t help. It reduces absorption by only 45% if given within that window. After that? Zero benefit. No point giving it. And don’t waste time on hemodialysis or whole bowel irrigation. Those don’t work for benzodiazepines. The 2023 update to StatPearls makes this clear: they’re not recommended.How Long Should You Monitor?
Symptoms usually fade in 12 hours. But not always.- Asymptomatic patients: Observe for at least 6 hours.
- Symptomatic patients: Monitor until fully alert, with normal breathing and reflexes.
- Elderly or those with liver disease: Can take 24 to 48 hours. Their bodies clear the drug slowly.
What’s Changing in 2025?
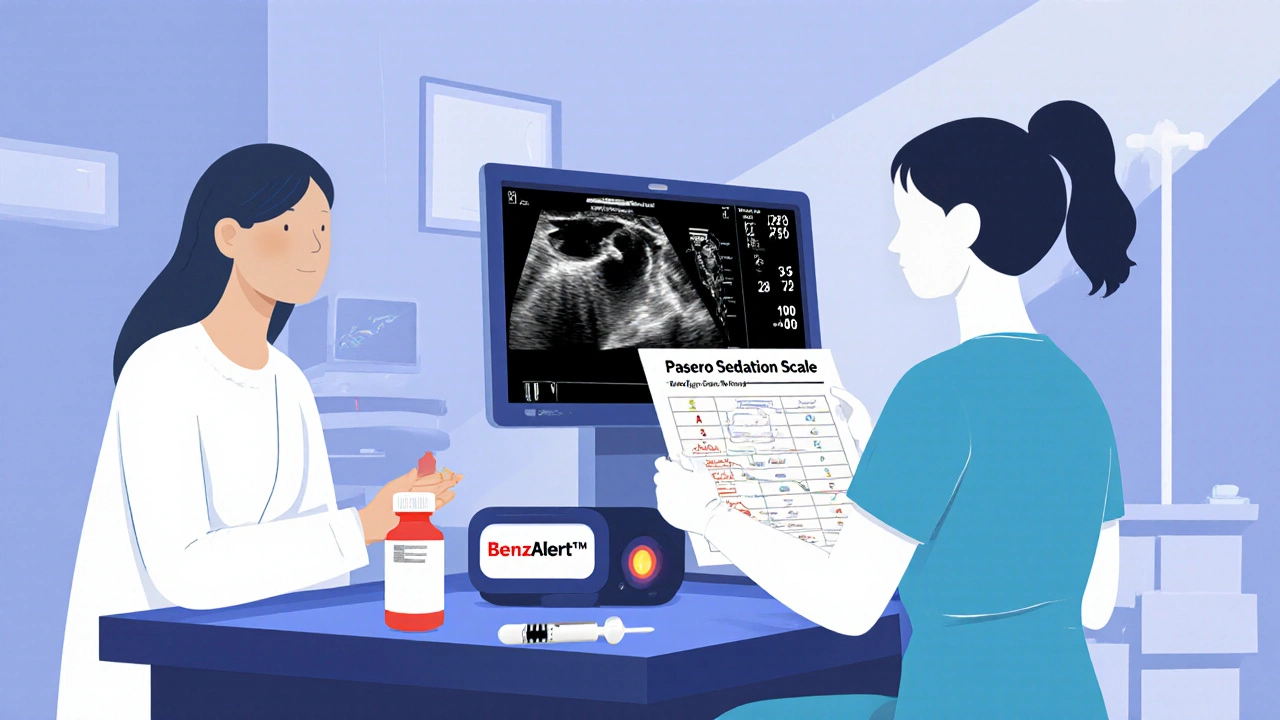
The tide is turning. The FDA now requires all benzodiazepine labels to warn about opioid interactions. The National Overdose Response Strategy spent $18.7 million in 2023 to train providers on spotting these combinations. New tools are coming. BenzAlert™, a blood monitor for benzodiazepine levels, showed 94.7% accuracy in trials. It’s not in hospitals yet-but it’s close. Point-of-care ultrasound (POCUS) is already helping. Instead of waiting for blood gases, ER teams use ultrasound to see if lungs are moving properly. One study showed it cuts intubation delays by 22 minutes. And harm reduction is expanding. As of 2023, 37 U.S. states include benzodiazepine recognition in naloxone distribution programs. That’s up from 12 in 2020. People are learning: if someone’s passed out and you have naloxone, give it. If they don’t wake up, they might still have a benzo overdose. You still need to call 911.What You Need to Remember
- Most benzodiazepine deaths happen with opioids or alcohol. Always assume co-ingestion.
- Flumazenil is rarely the answer. It’s risky and often unnecessary.
- Supportive care-airway, oxygen, monitoring-is the gold standard.
- Don’t discharge until ataxia is gone. Sedation fades faster than coordination.
- Illicit benzos are getting stronger. Etizolam and clonazolam are now the biggest threat.
When to Call for Help
If you suspect a benzodiazepine overdose:- Call emergency services immediately.
- Keep the person on their side if unconscious.
- Don’t try to make them vomit.
- Bring any pill bottles or packaging to the hospital.
- If you have naloxone and suspect opioids are involved, give it-but don’t assume it will fix everything.
Most people recover fully with proper care. But only if they get help in time.
Can you die from a benzodiazepine overdose alone?
Death from a pure benzodiazepine overdose is extremely rare-around 0.01% to 0.05%. Most fatalities occur when benzodiazepines are mixed with opioids, alcohol, or other depressants. The real danger is respiratory failure, not the drug by itself.
Is flumazenil safe to use in an emergency?
Flumazenil is rarely safe. It can trigger seizures in people with chronic benzodiazepine use-even if they’re not addicted. It also wears off quickly, so sedation can return. Most emergency departments no longer stock it. Supportive care is safer and more effective.
How long does a benzodiazepine overdose last?
Symptoms usually resolve in 12 hours. But in older adults or people with liver problems, it can take 24 to 48 hours. Coordination problems (ataxia) often last longer than drowsiness. Don’t discharge someone until they’re fully steady on their feet.
Why are illicit benzodiazepines more dangerous?
Illicit versions like etizolam and clonazolam are 3 to 10 times more potent than prescription benzos. They’re sold as fake Xanax pills, so users don’t know the dose. These drugs cause 68% of severe overdoses in the Western U.S. and are responsible for the recent spike in ER visits.
Should I give naloxone if someone overdoses on benzodiazepines?
Yes-if you suspect opioids are involved. Naloxone won’t reverse benzodiazepines, but it can save a life if opioids are also present. Many overdose deaths involve both drugs. Giving naloxone is low-risk and could be lifesaving. Always call emergency services regardless.
Can activated charcoal help in a benzodiazepine overdose?
Only if given within 60 minutes of ingestion. Benzodiazepines are absorbed quickly, so charcoal has no effect after that. Giving it later doesn’t help and wastes time. It’s not recommended in current guidelines.
What’s the biggest mistake in treating benzodiazepine overdose?
Missing co-ingestants. About 28% of cases involve opioids, alcohol, or other drugs that aren’t tested for. Assuming it’s just a benzo overdose leads to under-treatment. Always check for other substances before deciding on a treatment plan.
Are benzodiazepine overdoses becoming more common?
Yes. Between 2019 and 2022, prescriptions dropped by 14.3%, but overdose cases rose by 27%. That’s because illicit, high-potency benzos like etizolam are flooding the street market. Experts predict a 40% increase in ER visits by 2025.

Just saw a patient last week with etizolam toxicity-no history of benzo use, just bought ‘Xanax’ off Snapchat. Came in with GCS 6, respirations at 6/min. We didn’t even test for opioids at first. Turned out he’d been mixing it with fentanyl-laced weed. Charcoal was useless-6 hours out. We just intubated, gave O2, and waited. He woke up fine after 18 hours. Bottom line: assume co-ingestion. Always.
So let me get this straight-after all this ‘evidence-based’ nonsense, you’re still telling people to just ‘monitor’ someone who can’t breathe? No wonder ERs are overwhelmed. They’re treating overdoses like tea parties. Where’s the accountability? Where’s the punishment for these pill pushers? Someone needs to go to jail for this.
Okay but have you heard about the *real* story? The CDC quietly pulled flumazenil from all hospitals in 2022 because they found it was being used to cover up opioid deaths. The whole ‘it causes seizures’ thing? Total misdirection. Big Pharma doesn’t want you to have a real antidote because then people would stop using opioids and benzos together-and they’d lose billions. The FDA’s new labeling? A distraction. They’re not warning about interactions-they’re warning you not to trust your own instincts. I’ve seen it. I’ve seen the memos. They’re scared of what happens when people realize how easy it is to die from a pill they thought was safe.
And don’t get me started on ‘BenzAlert™’. That’s not a diagnostic tool-it’s a tracking chip. They’re building a database of every person who ever takes a benzo. Next thing you know, your insurance will deny you coverage if your blood levels are ‘too high’. This isn’t medicine. It’s control.
Thank you for this. I’m an EMT and we get these cases weekly. The hardest part is convincing families that their loved one isn’t ‘just sleeping’-they’re dying quietly. We always check for other drugs, even if they say ‘just Xanax’. You’d be shocked how often it’s something else.
👏👏👏 YES. This is the kind of post that makes me believe Reddit still has some brains left. Also-POCUS for respiratory assessment? GENIUS. I’ve been using it for months. No more waiting 20 mins for ABGs while someone’s brain turns to mush. And yes, naloxone first if you’re unsure. Free. Safe. Could save a life. 🤝💉 #SaveTheBreath
It’s fascinating how the medical community has quietly abandoned flumazenil while simultaneously promoting harm reduction strategies that are far more effective. The irony is delicious: we’ve spent decades pathologizing addiction, yet the most life-saving intervention is… patience and oxygen. Who knew the simplest tools were the most powerful? It’s almost poetic. The real villain isn’t the drug-it’s the belief that every problem needs a chemical solution.
While your clinical summary is technically accurate, it lacks the necessary epistemological rigor. You reference StatPearls as authoritative, yet it is a crowdsourced, non-peer-reviewed repository with no institutional accountability. The 68% statistic regarding illicit benzos in the Western U.S.? Source? Methodology? Confidence interval? Without these, you are merely propagating anecdotal consensus masquerading as evidence. Furthermore, you omit the fact that the rise in synthetic benzo overdoses correlates directly with the DEA’s 2021 scheduling of clonazolam-suggesting prohibition, not education, is the primary driver of adulterated supply. This is not medicine. It is policy theater.
How is it that in a country with such advanced medical infrastructure, we are still relying on ‘monitoring’ as a primary intervention? In the UK, we’ve had portable capnography in ambulances since 2017. We measure end-tidal CO2 in real time. We know when respiratory depression is worsening before the patient becomes unresponsive. Here? You wait for them to stop breathing. Then you intubate. This isn’t standard of care. It’s negligence dressed in white coats.
This is a dangerous and irresponsible piece of misinformation. You suggest that people should not use flumazenil under any circumstances, yet the FDA has approved it for emergency use since 1992. You are undermining the professional judgment of physicians who have successfully used it in controlled settings. Furthermore, your casual dismissal of activated charcoal is alarming. It has been used for over a century. To suggest it is ‘useless’ after 60 minutes is not only inaccurate-it is reckless. I am deeply concerned that laypersons will read this and delay seeking proper care. This is not helpful. It is harmful.
70% co-ingestion rate. 28% misdiagnosis. 0.7% flumazenil use. 68% illicit benzo overdoses. The numbers are consistent. The pattern is clear. This isn’t a medical crisis. It’s a behavioral epidemiological collapse. You treat the drug, not the context. The user isn’t a patient. They’re a data point in a failed public health model. And you’re still surprised when they die.
From a pharmacokinetic standpoint, the prolonged half-life of long-acting benzos (e.g., diazepam) in hepatic impairment necessitates extended observation windows beyond 24 hours. The Pasero Sedation Scale is underutilized in community EDs due to staffing constraints, but its sensitivity for detecting residual CNS depression is superior to subjective ‘appears awake’ assessments. Additionally, the emergence of clonazolam as a high-potency, low-molecular-weight analog significantly increases the risk of delayed respiratory depression due to its lipophilicity and tissue redistribution. Monitoring beyond 48 hours is not overcautious-it’s physiologically warranted in polypharmacy cases.
Flumazenil is not ‘rarely safe.’ It is precisely indicated in cases of pure benzodiazepine overdose in non-dependent patients. The 0.7% statistic is misleading-it reflects institutional bias, not clinical utility. In tertiary centers with full toxicology support, flumazenil remains a vital tool. To dismiss it entirely is to surrender to fear-based protocols. Medicine should not be dictated by liability concerns. It should be guided by physiology. And physiology tells us: when the drug is the sole agent, reversal is not only possible-it is appropriate.